Generality
Carbon monoxide (CO) poisoning is one of the most common causes of death from inhalation poisoning.
Carbon monoxide poisoning occurs in a subtle way; this gas, in fact, is colorless and odorless; moreover, the symptoms manifested by intoxicated individuals are rather non-specific and generic.

Causes
The causes of carbon monoxide poisoning can be different. Generally, among the most common we find:
- Malfunctions in domestic heating systems (such as, for example, boilers, coal or wood fireplaces, etc.);
- Malfunctions of wood or gas-fired appliances (such as, for example, the oven or gas water heaters);
- Fires;
- Malfunctions or inadequate ventilation inside cars.
Mechanism of Toxicity
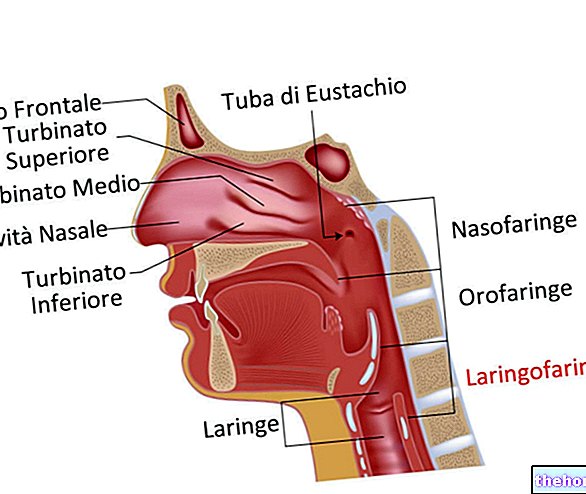
Carbon monoxide poisoning occurs above all when this dangerous gas accumulates in poorly ventilated environments. This poisoning also occurs in a subtle way, since CO is an absolutely colorless, odorless, tasteless and non-irritating gas; all these characteristics prevent to the individual to recognize the dangerous situation.
The carbon monoxide is then inhaled and rapidly absorbed in the lungs, thus entering the bloodstream.
The mechanism by which intoxication occurs is related to the ability of carbon monoxide to bind to hemoglobin - present in red blood cells - with a greater affinity than oxygen.
The CO, therefore, possessing a "high affinity for" hemoglobin (Hb), displaces the bond of oxygen with the aforementioned protein, leading to the formation of carboxyhemoglobin (COHb).
Carboxyhemoglobin, as you can easily imagine, is not able to release oxygen to the tissues as, instead, happens with hemoglobin. Furthermore, CO is able to bind to a particular enzyme involved in the cellular respiration mechanism: the cytochrome tissue oxidase, thus preventing cells from using the remaining oxygen.
To summarize briefly, carbon monoxide causes toxicity through the following mechanisms:
- Bond with hemoglobin leading to the formation of carboxyhemoglobin;
- Impaired ability of hemoglobin to deliver oxygen to tissues and organs;
- Inhibition of tissue cytochrome oxidase.
The combination of all these mechanisms leads to the lack of supply and use of oxygen, which results in the onset of various non-specific symptoms that characterize carbon monoxide intoxication.
Diagnosis
Often, the diagnosis of carbon monoxide poisoning is difficult to make, precisely because of the subtle way in which it is established and because of the non-specific symptoms.
If the doctor suspects a possible carbon monoxide intoxication, he will immediately carry out blood tests to evaluate the blood levels of carboxyhemoglobin, in order to identify the actual presence and severity of the intoxication.
In addition to this, to confirm the diagnosis, the doctor may resort to performing other tests, such as blood gas analysis and pulse oximetry.
In the most severe intoxications, to assess the extent of the damage caused by carbon monoxide intoxication, the doctor may also decide to perform tests such as electrocardiogram, CT scan, magnetic resonance and electroencephalogram.
Symptoms
For further information: Symptoms Carbon monoxide poisoning "
As mentioned, the symptoms induced by carbon monoxide poisoning are rather non-specific and involve different body areas. However, these symptoms are all related to the poor supply of oxygen to the various organs and tissues, which occurs during this particular type of d "intoxication.
Symptoms that can occur in the initial phase of carbon monoxide poisoning consist of:
- Nausea;
- He retched;
- Headache;
- Weakness;
- Asthenia;
- Dizziness;
- Dyspnea on exertion;
- Chest pain;
- Tachypnea;
- Confusion and disorientation;
- Irritability;
- Difficulty concentrating
- Tachycardia;
- Heartbeat.
If carbon monoxide poisoning is severe, there may also be:
- Convulsions;
- Disturbances of sight and hearing;
- Drowsiness;
- Ataxia;
- Hypotension;
- Generalized muscle stiffness;
- Cardiocirculatory arrest;
- Respiratory failure;
- Loss of consciousness;
- Coma and, in severe cases, death.
Furthermore, it should be remembered that sometimes - days or even weeks after the intoxication - late symptoms may occur, such as:
- Dementia;
- Parkinsonism;
- Psychosis;
- Mnesic alterations.
Types of "Intoxication
Carbon monoxide poisoning can be classified according to their severity, which is closely related to the levels of carboxyhemoglobin present in the patient's blood.
In this regard, we can distinguish:
- Suspected intoxication, characterized by blood carboxyhemoglobin levels of 2-5%. However, in these cases of suspected intoxication, it should be remembered that smoking patients have higher carboxyhemoglobin levels than non-smoking patients.
- Mild intoxication, in this case the blood carboxyhemoglobin levels are 5-10%; this intoxication is characterized by decidedly nonspecific symptoms, such as headache, generalized malaise and nausea.
- Moderate intoxication, in which blood carboxyhemoglobin levels increase to 10-25%; in this case, the symptoms that may occur are more marked and consist of: intense headache, dizziness, visual disturbances, retinal haemorrhages, intense red coloring of the mucous membranes, hypotension and tachycardia.
- Severe intoxication, in which blood carboxyhemoglobin levels are above 25-30%. In these cases, the symptoms are very serious and include convulsions, coma, respiratory failure, cardiac arrest and death.
First Aid and Treatment
First aid intervention, as well as inpatient treatment of carbon monoxide poisoning, are essential to safeguard the patient's life and preserve him from the onset of permanent damage.
The task of the rescuers is basically that of immediately removing the patient from the source of carbon monoxide and supporting his vital functions until he reaches the hospital center, at which all necessary analyzes and treatments will be performed.
In particular, the treatment of carbon monoxide poisoning involves the administration of 100% oxygen to the patient. In fact, very high concentrations of oxygen are able to reduce the half-life of carboxyhemoglobin, both in the blood and in the tissue. More specifically, the patient can be subjected - depending on the case and depending on the doctor's opinion - to two different types of treatment:
- Normobaric oxygen therapy, consisting in the administration of 100% oxygen through the use of a special face mask. By doing so, the half-life of carboxyhemoglobin is reduced to 60-90 minutes, compared to the 2-7 hours that would be necessary without the administration of oxygen.
Usually, this type of treatment is continued until the carboxyhemoglobin levels are below 5%. - Hyperbaric oxygen therapy, consisting in the administration of 100% oxygen in a hyperbaric chamber in which the pressure is higher than the atmospheric one (indicatively, 2.5-3 atmospheres). In this case, the half-life of carboxyhemoglobin - both in the blood and in the tissues - is drastically reduced to 30 minutes.
However, it should be remembered that hyperbaric oxygen therapy can only be undertaken in certain cases and that it is really effective only if it is performed as soon as possible after carbon monoxide poisoning (approximately, within 12 hours).