Dental abscess: introduction
The diagnosis of dental abscess is quite easy, often a simple medical history (collection of symptoms reported by the patient) is sufficient.The subject affected by dental abscess accuses an unstoppable, throbbing and acute toothache, such as to hinder chewing or - even worse - normal daily activities and night rest.

The prognosis is excellent when the dental abscess is stopped as soon as the first symptoms appear; otherwise, in case of non-intervention, the dental abscess can cause devastating effects, even death in extreme cases.
Diagnosis
As mentioned, the diagnosis of a dental abscess is quite simple. An anamnestic investigation (ie the collection of the symptoms accused by the patient) is in fact sufficient to hypothesize a dental abscess in progress. In any case, the dentist proceeds with a specialist visit to verify the infection. The presence of purulent material (bacteria, cellular debris, plasma and white blood cells) in the gum, in the jaw bone or in the pulp of the tooth can be ascertained by means of appropriate diagnostic-investigative tests:
- Touching the tooth. Many times, dental abscesses make the teeth extremely sensitive; therefore, a simple brushing of the tooth can exacerbate the toothache. To test the intensity of the pain, the dentist gently touches or presses lightly on the tooth involved in the pathology.
- Aspiration: the dentist inserts the needle of a syringe into the inflamed gum area to aspirate any pus sample. Subsequently, the sample is sent to the laboratory for bacterial culture examination.
- Radiography: diagnostic test useful for detecting the severity of the dental abscess. Radiographs are generally indicated in case of broken and chipped teeth, and hypothetical infection of the jaw bone.
Therapies and treatments
Dental abscess therapy aims to:
- Kill the pathogens involved in the infection → antibiotics
- Remove pain and all other symptoms → therapeutic aids
- Saving the tooth from a "hypothetical extraction → immediate intervention
Since it is an infection, a targeted antibiotic treatment is the most appropriate therapy to effectively eradicate the dental abscess. Often, however, alongside the antibiotic treatment it is necessary to incise the dental abscess to drain its contents. The dentist, with the help of sterile instruments, first of all proceeds to anesthetize the area to be treated; then, the doctor makes a small incision in the abscess to remove the accumulated purulent material.
To combat the inevitable pain that accompanies the dental abscess, the doctor prescribes the patient anesthetic-pain relieving drugs (eg ibuprofen, naproxen, acetylsalicylic acid). In the presence of high fever, the most suitable drug is paracetamol.
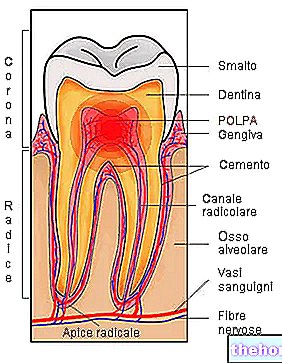
The most effective solution for a PERIAPICAL ABSCESS (irreversible pulpitis) is the devitalization of the tooth, which avoids an "eventual extraction. This intervention consists in the removal of the damaged dental pulp, and in its subsequent filling with special amalgams or biocompatible materials. Subsequently, the tooth must be reconstructed: metal and carbon posts can be implanted (to support the reconstruction) and, finally, it is possible to cover the tooth with a capsule.
If the devitalization procedure was not performed correctly, the dental abscess could create greater damage. In such circumstances, it is necessary to proceed with a "surgical extraction of the diseased tooth.
A PERIODONTAL ABSCESS generally requires less invasive therapies than in the previous case. Detartarsai (surgery that involves the professional removal of tartar and plaque), supported by antibiotic and pain-relieving therapy, is sometimes sufficient to cure the dental abscess. Other times, after having carefully cleaned the gingival pocket in which the " abscess, it is necessary to reshape the gum tissue to minimize the risk of recurring infections.
Prognosis
The prognosis of a tooth abscess is excellent when the infection is carefully treated during the first stage (very early symptoms) with drainage and antibiotic therapy.
Conversely, when left untreated, dental abscess can cause very serious complications, such as fistulas, cysts, granulomas, tooth loss, osteomyelitis, infection of the floor of the mouth and septicemia (sepsis). In diabetic, cancer and severely immunocompromised patients, an untreated tooth abscess can give a poor prognosis (patient death).
Prevention
Careful daily oral hygiene, accompanied by professional scaling every 6-12 months, prevents cavities and diseases of the oral cavity in general, including dental abscesses.
For proper oral hygiene it is necessary ...
- Brush your teeth at least three times a day, preferably immediately after each meal or snack
- Use quality toothpastes
- Alternate whitening (harsh) toothpastes with gentler toothpastes to prevent wearing down tooth enamel
- Floss at least once a day
- Rinse your mouth with antiseptic and fluoride-enriched mouthwashes
- If possible, use a soft-bristled or electric toothbrush
Periodic check-ups by the dentist can surprise any infections that are still asymptomatic in the bud; therefore, timely intervention on caries, gingivitis or periodontitis (pyorrhea) minimizes the risk of complications by avoiding the appearance of dental abscesses.
Other articles on "Dental Abscess: Diagnosis, Therapy and Prognosis"
- Dental Abscess: Causes and Symptoms
- Remedies for Dental Abscess