What is pulpitis?
Pulpitis is an inflammatory process of the dental pulp which, in jargon, is called "nerve inflammation of the tooth.'
To understand...
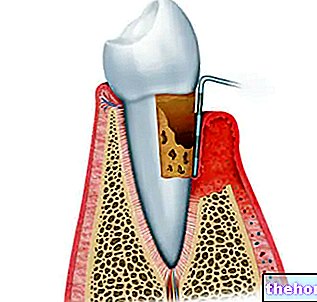
The dental pulp is the innermost part of the tooth, rich in nerve endings, arterioles, venules and odontoblasts (cells used for the production of dentin).

Treatment of pulpitis consists of minimizing symptoms (pain) and removing the cause responsible for the inflammatory process. The cure for pulpitis is relatively simple; however, when the inflammation is not carefully treated, the tooth can undergo a degenerative-necrotic process (losing its vitality). In such circumstances, pulpitis requires devitalization, partial pulp removal or tooth extraction.
Causes
In most cases, pulpitis is the immediate consequence of cariogenic damage. Caries is a destructive process of the tooth that causes the progressive demineralization of enamel and dentin.The bacteria present in the oral cavity, greedy for sugars, produce acid substances starting from the fermentation of carbohydrates: it is these acid products that pierce the enamel, reaching the dentin and attacking the pulp of the tooth until they trigger pulpitis.
Fermentation of sugars by bacteria of the oral cavity → production of acid substances that pierce the enamel → propagation of damage to the dentin level → caries affects the dental pulp → pulpitis
In addition to caries, pulpitis can originate from:
- Trauma to the teeth
- Periodontitis (or pyorrhea)
- Repeated invasive dental interventions
- Thermal insults derived from dental procedures (e.g. laser whitening with CO2 lamps)
- Bruxism
- Dental malocclusions
- Incorrect chewing
- Poor oral hygiene
Symptoms and classification
For further information: Pulpitis Symptoms
The characteristic symptom of pulpitis is toothache, usually very intense, acute and throbbing, which can be persistent or intermittent. Most of the time, in the presence of pulpitis, the patient accuses a fierce pain in the teeth which, however, is difficult to locate in a precise point.
In almost all of the pulpits, the pain is aggravated by different kinds of stimuli, such as chewing, hot / cold and sugary foods (especially chocolate).
Please Note
In the very early stages of the disease, pulpitis can be asymptomatic. For this reason, the annual check-up by the dentist is essential for early diagnosis of any dental disorders (such as pulpitis). In such circumstances, it is therefore possible to act accordingly with timely treatment before the symptoms become unbearable and the damage irreversible.
According to the degree of inflammation and the depth of the pulp lesion, two forms of pulpitis are distinguished:
- REVERSIBLE PULPITIS: it is an "inflammation moderate of the dental pulp which, if treated early and appropriately, retains its healing capacity. The pain that characterizes reversible pulpitis - accentuated by heat or cold, chewing or sugary foods - disappears immediately after the stimulus is removed.
- IRREVERSIBLE PULPITIS: occurs when reversible pulpitis is not treated in time. The irreversible form is characterized by an extremely severe "pulp inflammation, accompanied by a degenerative process that progressively evolves into necrosis of the dental pulp. Inadequately treated pulpitis can cause abscess, periodontitis, granuloma or cyst. Toothache associated with irreversible pulpitis. it persists even after the removal of mechanical (chewing), chemical (sugar) or thermal stimuli.
Pulpitis: care
A "shock" treatment is essential to prevent pulpitis from degenerating into its irreversible form.
Pulpitis treatment uses:
- Analgesic drugs to relieve pain
- Medical strategies aimed at removing the cause of pulpitis
First of all, pain can be managed by administering pain relieving drugs, which can mask the symptoms and relieve the patient. While paracetamol and NSAIDs are usually sufficient to effectively relieve mild to moderate pain, codeine or other opiates are needed for unmanageable and severe pain.
Alongside the drug treatment, the dentist proceeds with medical treatment, consisting of a specific intervention to remove the cause of the pulpitis. When pulp involvement is limited, pulpitis must be treated simply by eliminating the caries. Otherwise, in the presence of severe inflammation and pulp necrosis, it may be necessary to partially or totally remove the pulp of the tooth (devitalization or eventual removal of the tooth).
Prevention
The best cure for pulpitis is prevention. Given that most of the pulpits are the consequence of cariogenic processes, the adoption of some simple dietary precautions, combined with the correction of an incorrect lifestyle, can prevent the onset of pulpitis.
To minimize the risk of pulpitis it is necessary ...
- Take care of your teeth daily:
- Brush your teeth at least three times a day with suitable toothpastes. Toothpastes containing fluoride are the most suitable for preventing pulpitis because they strengthen the dental enamel
- Brush your teeth from the gum towards the tooth, never the other way around
- Limit the use of toothpastes formulated with abrasive whitening products, which can damage the enamel, thus favoring tooth decay and pulpitis
- Floss at least once a day
- Replace the toothbrush every 2-3 months
- Use anti-plaque mouthwashes
- Limit the consumption of sweets and sticky foods - such as jam, honey and chocolate - which can adhere to the enamel and favor the entry of bacteria
- Undergo periodic check-ups at the dentist, at least once or twice a year. Routine visits can surprise any inflammatory processes that are still asymptomatic in the bud, including pulpitis, and remedy them before the damage becomes irreversible.