What is periodontitis?
By Prof. Filippo Graziani
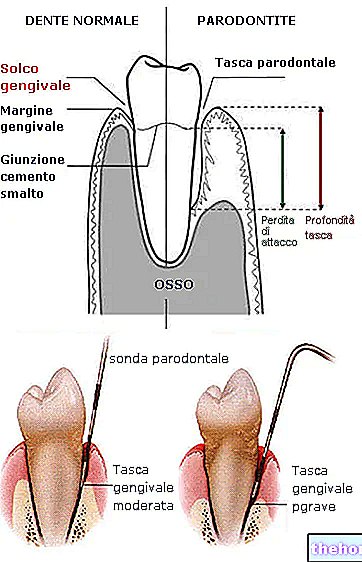
Periodontitis is an inflammatory disease that affects the supporting tissues of the tooth (the gum, the periodontal ligament, the cementum of the root and the bone).
The main feature of periodontitis is the destruction of the supporting tissue of the tooth, which is measured through a parameter called loss of clinical attachment.
Watch the video
- Watch the video on youtube
Loss of attachment results in gum pockets, receding gums, and alveolar bone loss. There is also gum bleeding, due to inflammation of the gums.
Periodontitis is one of the most common chronic diseases in the world:
- 11% of the world population is affected by severe periodontitis
- 50% of people over 30 suffer from some gum problem
- The likelihood of developing periodontitis increases after the age of 30, with a peak of new cases between the ages of 35 and 40.
- With increasing age, the likelihood of developing severe forms of periodontitis increases, affecting more than 30% of people over the age of 60.
Since 2017, a new staging and classification system for periodontal diseases and conditions has been in use, very similar to that used in oncology. This system makes it possible to diagnose periodontitis by understanding the severity of the disease and its management complexity (stage I - IV), but also by considering additional information on the biological characteristics of the disease, such as the rate of progression and the risk for the patient (grade A - C). Depending on the number of teeth affected by the disease, periodontitis can be defined as localized (less than 30% of the affected teeth) or generalized (more than 30% of the affected teeth).
Untreated periodontitis results in tooth loss, causing progressive partial edentulism, which can lead to impaired chewing function. Therefore, periodontitis cannot be considered a localized disease that affects only the mouth, as it also compromises the aesthetics of the smile, nutrition, quality of life and self-esteem, as well as imposing the socio-economic burden of treatment. dental.
What Causes Inflammatory Periodontal Diseases?
Periodontitis is a multifactorial inflammatory disease, that is, caused by multiple factors.
The main causative factors are certain pathogenic, anaerobic and gram-negative bacteria found in the biofilm above and below the gums. It is therefore a disease caused by bacteria, but not infectious - in fact, although it is caused by bacteria, it is technically not contagious.
The inflammatory response to the accumulation of bacteria, and therefore the susceptibility to the disease, is altered by the so-called risk factors. These factors are divided into 2 groups: modifiable risk factors (which can be influenced and controlled) and non-modifiable risk factors (which cannot be controlled.) Risk factor management is an essential part of the prevention and treatment of periodontal disease.
GENETIC BACKGROUND
Familiarity - disease common in the family
Genetic variations - polymorphisms (IL-1; PgE, etc.)
DEMOGRAPHICSAge
SYSTEMIC CONDITIONS AND PATHOLOGIES
Pre-Diabetes
Diabetes
Obesity
Hormonal changes (puberty, pregnancy, menopause)
Medicines
Depression of the immune system (for example due to diseases such as HIV)
Frequent viral infectionsHABITS OF LIFE
Poor oral hygiene
Smoke
Diet
Stress and other contributing psychological factors
Consumption of alcoholPeriodontitis develops from gingivitis. Gingivitis is defined as inflammation of the gums, without bone loss, which if treated in time is reversible. The longer the gingival inflammation persists and is not controlled, the higher the chance that gingivitis will progress to gingivitis in susceptible people. periodontitis. However, it is important to point out that not all cases of gingivitis will develop into periodontitis and not all people with gingivitis will develop periodontitis.
Various factors can contribute to the progression of periodontitis:
Pathogenic (disease causing) bacteria within the biofilm.
- Poor oral hygiene habits and lack of professional care.
- Incorrectly placed fillings or teeth, which trap and hold the biofilm.
- Some drugs that lead to an increase in the inflammatory response of the gums.
- Local risk factors: inadequate dental restorations (overflowing fillings, crowns and bridges).
Systemic diseases and periodontitis
Despite being a disease of the oral cavity, periodontitis is linked to general health conditions. Currently, periodontitis is associated with 57 systemic diseases that apparently have no connection with the mouth, such as rheumatoid arthritis, Alzheimer's disease, chronic kidney disease, bronchopneumopathies and diseases associated with pregnancy (such as preeclampsia and preterm birth), etc.
In particular, two very common diseases have been associated with periodontitis: atherosclerotic cardiovascular disease and diabetes.
Atherosclerotic cardiovascular disease and periodontitis
CVD (cardiovascular diseases) is an umbrella term that refers to a wide variety of diseases and conditions involving the heart and blood vessels. Atherosclerotic vascular diseases are the leading cause of death worldwide; among these, ischemic heart disease and stroke are the most frequent causes of mortality among all CVDs. Scientific evidence suggests that the increase in systemic inflammation may be associated with the increase in the thickness of the artery walls, which then can lead to CV events. Chronic inflammatory diseases such as rheumatoid arthritis, psoriasis and chronic bowel disease have all been associated with an increased risk of future CV events. Research has shown that periodontitis is also one of the diseases chronic inflammatory diseases most common in the world, can be considered a risk factor for CVD.
- Periodontitis increases the risk of atherosclerosis and endothelial dysfunction.
- It can lead to cerebrovascular events, such as transient ischemic attack or stroke, but also cardiovascular events such as angina, heart attack and heart failure.
- Individuals with moderate periodontitis are 20% more likely to develop hypertension, while those with severe periodontitis are up to 49%.
However, non-surgical causal periodontal treatment is also beneficial in terms of cardiovascular health. This is indicated by the reduction of heart attack risk and systolic blood pressure, improvement of endothelial function, lipid profile and arterial stiffness.
Diabetes and periodontitis
Diabetes, like periodontitis, is one of the most common chronic diseases in the world, affecting more than 420 million people. 90% of diabetics have type 2 diabetes, due to the ineffective use of insulin by the body. This type of diabetes is mainly the result of excess body weight and lack of physical activity. Inflammation, which is involved in the pathogenesis of both diabetes and periodontitis, is the link between the two diseases. Their relationship between these two diseases is bidirectional: those with diabetes are more likely to be affected by periodontitis and those with periodontitis have more risk of getting diabetes.
- People with diabetes are more likely to develop periodontitis - in particular, periodontitis is considered the 6th complication of diabetes.
- Patients with type II diabetes with periodontitis have worsening glycemic control and a greater degree of complications
- People with type II diabetes and periodontitis tend to develop more complications than periodontally healthy diabetics (such as retinopathies, macroalbuminuria and kidney disease).
- Patients with uncontrolled diabetes have a worse response to periodontal treatment- individuals with periodontitis are 30% more likely to develop type 2 diabetes than those who are periodontally healthy
- the more severe the periodontitis, the more inadequate glycemic control is, as indicated by "increased" HbA1c, impaired glucose tolerance (or metabolic syndrome) and prevalence of pre-diabetes.Scientific evidence underlines the ability of non-surgical periodontal treatment to reduce glycated hemoglobin (HbA1C) by 0.4%. An "important reduction equal to that of a second hypoglycemic drug. For this reason the European Federation of Periodontology and the International Diabetes Federation have drawn up joint guidelines.
Periodontitis and systemic diseases: the link between them
As already mentioned, bronchopneumopathies, rheumatoid arthritis, chronic kidney disease, Alzheimer's disease and some diseases associated with pregnancy (such as pre-eclampsias and preterm birth) are just some of the systemic diseases associated with periodontitis.
There are two mechanisms that explain the connection between the oral cavity and the rest of the body: bacteremia and systemic inflammation.
- the bacteria of the dental plaque penetrate the epithelium of the gingival sulcus, up to the gingival connective tissue. From there the bacteria then enter the bloodstream through the microcirculation.
- Bacteremia occurs daily during the most common procedures, such as tooth brushing. However, the type and number of bacteria are different between a healthy individual and a person with periodontitis.
- the accumulation of biofilm in the gingival sulcus determines a local inflammatory response, characterized by the production of molecules that favor inflammation - cytokines and interleukins, which trigger a systemic inflammatory response starting from the liver
- people with periodontitis show higher systemic levels of inflammatory molecules than unaffected people
- a persistent chronic inflammatory state, even if minimal, is associated with the onset of numerous systemic pathologiesGingival inflammation
In a "healthy" individual, the inflammatory processes in the body are well controlled and balanced through natural healing pathways.
In general, the presence of microbes or lesions triggers a self-defense reaction of the body, represented by an inflammatory and immune response. Once the causative agent is removed through these responses, balance is restored. Acute (short-term) inflammation is therefore considered a positive thing, a normal evolutionary protective mechanism. However, in periodontal inflammatory diseases, ie gingivitis and periodontitis, the causative factor (the bacterial biofilm) is continuously present above and below the gums; this causes a constant state of alertness of the organism, which determines a chronic and long-term inflammatory state.
In susceptible people these responses are further altered. Therefore, in the event of a percentage increase of the most pathogenic bacteria in the bacterial biofilm, destructive processes can occur which manifest themselves as tissue loss, i.e. periodontitis.
Each symptom of inflammation has its own function.
Further reading
Genco, R. J., & Borgnakke, W. S.. Risk factors for periodontal disease. Periodontology 2000, 62, 59–94. https://doi.org/10.1111/j.1600-0757.2012.00457.x
Graziani, F. (2020, January 20). Periodontitis: Does gum disease increase your risk of hypertension, heart attack and stroke? Open Access Government. https://www.openaccessgovernment.org/gum-disease-increase-hypertension-heart-attack-stroke/81055/
Graziani, F., Gennai, S., Solini, A., & Petrini, M.. A systematic review and meta-analysis of epidemiologic observational evidence on the effect of periodontitis on diabetes An update of the EFP-AAP review. Journal of Clinical Periodontology, 45, 167–187. https://doi.org/10.1111/jcpe.12837
Hasturk, H., & Kantarci, A.. Activation and Resolution of Periodontal Inflammation and Its Systemic Impact. Periodontology 2000, 69, 255-273. https://doi.org/10.1111/prd.12105
Sanz, M., Ceriello, A., Buysschaert, M., Chapple, I., Demmer, RT, Graziani, F., Herrera, D., Jepsen, S., Lione, L., Madianos, P., Mathur , M., Montanya, E., Shapira, L., Tonetti, M., & Vegh, D.. Scientific evidence on the links between periodontal diseases and diabetes: Consensus report and guidelines of the joint workshop on periodontal diseases and diabetes by the International diabetes Federation and the European Federation of Periodontology. Diabetes Research and Clinical Practice, 137, 231–241. https://doi.org/10.1016/j.diabres.2017.12.001
Sanz, M., Marco del Castillo, A., Jepsen, S., Gonzalez ‐ Juanatey, JR, D "Help, F., Bouchard, P., Chapple, I., Dietrich, T., Gotsman, I., Graziani, F., Herrera, D., Loos, B., Madianos, P., Michel, J., Perel, P., Pieske, B., Shapira, L., Shechter, M., Tonetti, M., … Wimmer, G. Periodontitis and cardiovascular diseases: Consensus report. Journal of Clinical Periodontology, 47, 268–288. https://doi.org/10.1111/jcpe.13189