Hepatitis A
Hepatitis A is a type of viral infection that affects the liver, which is sporadic in Europe, but is quite common in other parts of the world, such as, for example, Africa and India.

The initial symptoms of hepatitis A generally show up within two months and are similar to those of the flu; include: fever (usually not exceeding 39.5ºC), joint and muscle pain, feeling sick and tired, and diarrhea.
These can be followed by other related symptoms, such as: jaundice, dark urination and pale stools, itching, swollen and tender liver. Adults and the elderly tend to have more severe manifestations. In most cases, the liver fully regains overall function.
The correlations between diet and hepatitis A are of two types:
- Diet as a means of contagion
- Diet for the functional recovery of the organ and support during healing.
Diet and Contagion
In Italy, hepatitis A is mainly contracted by eating raw foods, sometimes live, such as bivalve molluscs (mussels, oysters, clams, cockles, etc.); these, contaminated by sewage (often abusive), can induce infection.
Contagion can also occur through the ingestion of contaminated water (from groundwater polluted by discharges on the ground) or raw vegetables, irrigated with polluted water (rivers, canals, waste, etc.).
In 2013, in Italy and other European countries there was an "epidemic of hepatitis A associated with the consumption of frozen berries from Eastern Europe".
Diet in case of Hepatitis A
Since the liver is an organ responsible for a multitude of different functions, its impairment in case of hepatitis can be quite debilitating. Among other things, this organ is responsible for secreting bile juices aimed at digestion. It synthesizes various plasma proteins intended for the transport of lipids in the blood (lipoproteins). In addition, it deals with the metabolism of most circulating molecules, from nutrients to drugs.
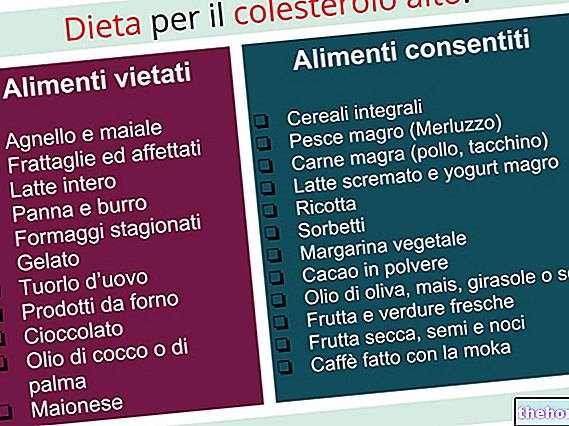
To reduce the load on the liver and facilitate the remission of hepatitis A, it is necessary to follow some basic dietary rules:
- Abolition of ethyl alcohol: when necessary, this is the most important change for those diagnosed with hepatitis
- Elimination of junk food and drinks or junk-food: as they are rich in saturated or hydrogenated fats (with trans-conformation chains), refined sugars, food additives (sweeteners, preservatives, etc.) and toxic molecules deriving from combustion (acrylamide, formaldehyde, acrolein , polycyclic aromatic, etc.). Among the junk foods we mention:
- packaged sweet and savory snacks, potatoes and other fried foods, hamburgers and other fast-foods, sweet drinks (carbonated or not), coffee, etc.
- Limit refined foods: many processes such as, for example, the refining and bleaching of flour, are based on physical and chemical mechanisms that deplete the food of fiber, vitamins and minerals (up to 78%). Remember that many vitamins are factors coenzymatics necessary to support very important cellular processes; however, these are often stored in the liver which, if suffering, could perform its function incompletely.
- Avoid excessive meals or prolonged fasts beyond 12-14 hours. The liver is responsible for glycemic maintenance which, in the case of fasting, requires a significant metabolic effort for neoglucogenesis starting from amino acids.
- In the case of celiac disease, meticulous abolition of gluten: this should be excluded regardless of hepatitis A. In fact, it is harmful for the intolerant, in which it causes an increase in the inflammatory state. It is absolutely necessary that, in the case of hepatitis A, celiacs take care of dietary hygiene by eliminating even the smallest exposure to cereals and derivatives containing gluten (wheat, spelled, spelled, rye, barley, oats and sorghum).
- Do not drink tap water, if of dubious quality: it is a problem that arises mainly when the source is not drinkable; heavy metals and toxic inorganic chemicals may be present, all compounds that the diseased liver is unable to process optimally.
- Eliminate unnecessary medications and dietary supplements.
- Consume fruit and vegetables in abundance: consume them at every meal; being able to choose, place fruit at breakfast and in secondary snacks, avoiding inserting it at lunch and dinner in order not to increase the glycemic load too much (since cereals and legumes are already present).
- Use food of vegetable origin with the following characteristics: fresh, better if “alive” and from agriculture that respects a rigid disciplinary. It is advisable, if possible, not to deprive them of the peel.
- Promote the intake of molecules useful for the liver: among these, all the vitamins with antioxidant function stand out (provitamin A, vitamin C, vitamin E) and the other molecules that intervene in a similar way (zinc, selenium, phenolic substances, chlorophyll, etc. Moreover, there are foods that contain active hepato-protective ingredients; the main ones are artichoke and milk thistle, thanks to the contribution of cynarin and silymarin.
- Increase the fraction of polyunsaturated fats (both essential omega 3 and omega 6, and non-essential such as omega 9) to the detriment of others; the most recommended foods are: oily fish (mackerel, mackerel, bonito, anchovies, sardines, etc.), cold-pressed vegetable oils (extra virgin olive oil, linseed, walnut, etc.) and oil seeds (almonds, sesame, etc.).
Other articles on "Diet and Hepatitis A"
- Medicines for the Treatment of Hepatitis A
- Hepatitis A
- Hepatitis A: risk factors, diagnosis and treatment
- Hepatitis A: vaccine and prevention







.jpg)


















