In reality, the only allergic form that can occur as a result of the intake of milk and derivatives has nothing to do with lactose, since it concerns the proteins of these foods.
In this regard, it would also be appropriate to make a distinction between the different allergic forms, those towards cow's milk proteins, breast milk (very difficult to treat) etc. But perhaps it is better not to put too much meat on the fire; for the moment we will simply limit ourselves to shedding more light on these two apparently similar and actually completely different disorders.
L "intolerance to lactose and allergy to milk proteins are very vast and difficult to summarize in a few lines, therefore, we will try to focus only on some fundamental concepts for basic understanding.
and metabolic reactions quite different from each other.
Food intolerance
It is a NON immune-mediated reaction (ie it is outside the mechanisms of the immune system); intolerances include: enzymatic deficiencies (such as the lack of intestinal lactase due to lactose intolerance), metabolic and food poisoning. They can be linked to pharmacological properties (caffeine in coffee), to the release of histamine, to individual susceptibility to particular enzymatic deficits or to idiosyncratic phenomena. The intolerance reaction is always linked to the quantity of food ingested and the complications are limited to the gastrointestinal tract.
Food allergy
It is "an adverse reaction to food or nutrients triggered by the immunological mechanism; allergic immunological reactions are of two types: Immuno Globuline E (IgE) MEDIATED and NON IgE mediated, and can cause both systemic and localized manifestations, limited to the gastro tract -intestinal, cutaneous or respiratory The most serious complication of the allergic reaction is anaphylactic shock.
Allergens most frequently responsible for food allergy
- Cow's milk proteins (a-lactalbumin, B-lactoglubin, casein)
- Eggs (egg white and yolk);
- Fish;
- Soy;
- Grain;
- Peanuts.
The diagnostic process to differentiate "allergy or" intolerance can be very complex and, especially in children, must follow a well-determined path; it is a diagnosis that is often complicated by the high number of triggering mechanisms and the quantity of food ingested with the diet NOT included in the diagnostic tests.
) is a disorder that occurs after the intake of lactose (a disaccharide carbohydrate contained in milk and dairy products) only in subjects who do not have a sufficient quantity of lactase (a specific enzyme of intestinal cells responsible for breaking down lactose into glucose + galactose).
Lactose undigested by lactase becomes a substrate for fermentation of the intestinal bacterial flora in the large intestine, with the relative production of: carbon dioxide (CO2), hydrogen ions (H2), methane (CH4) and organic acids; this condition causes an abnormal increase in intestinal motility and triggers symptoms of: swelling, flatulence and often also foamy diarrhea.
L "intolerance to lactose is less common in the countries of NORTH Europe (whose populations have kept the consumption of milk and dairy products high), while it occurs more frequently in Asia, Africa and South America (countries in which little milk and milk are consumed). derivatives).
The pathology can be diagnosed thanks to an examination called the H2 breath test; it is an "analysis of EXPIRED gases after having taken a certain amount of lactose.
Regarding the diagnosis, we remind you that lactose intolerance is a disorder that manifests itself with extreme variability; it can be present and symptomatic, present but asymptomatic and there may even be cases of strong symptoms but with negative H2 breath test results (none alteration of gases).
Note: A correlation has recently been observed between improvement of symptoms and integration / reconstitution of the intestinal probiotic bacterial flora.
vaccine, voluntarily omitting that of human milk since, although it represents a very serious disorder, it is characterized by a more limited prevalence and "incidence.
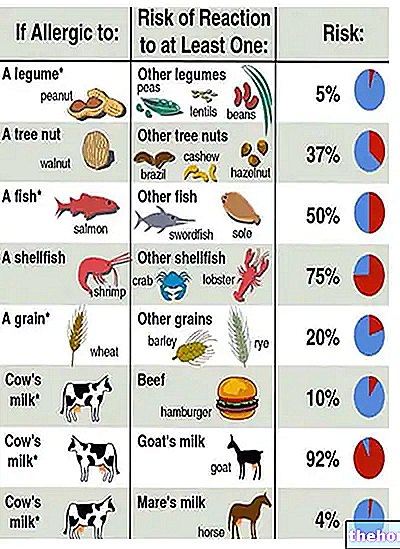
Cow's milk allergy is the most common allergic form in children (who have greater intestinal permeability) and the fifth in adults; probably, the difference in prevalence and incidence between the two age groups is justifiable by a real improvement in tolerability to this potential allergen. Cow's milk protein allergy manifests itself with abdominal pain, diarrhea and vomiting, therefore, it constitutes the first element of differential diagnosis from lactose intolerance.
The antigen that most frequently generates the adverse reaction is the protein beta-lactoglobulin, then comes the alpha-lactalbumin and finally caseins; it is however possible that the subject manifests sensitivity even to several proteins at the same time.
The pathological mechanism is triggered by the recognition of the protein by the white blood cells which release some specific antibodies (IgE) that adhere to the antigen; in this way (and thanks to the intervention of other specific cells: Mast cells and T lymphocytes) a kind of antigen storage and preparation by the immune system.
The second contact between the antigen and the immune system generates the allergic reaction.
There are many proteins contained in different types of milk (human, goat, etc.) capable of generating allergy, therefore, the only way to make this food harmless for the nutrition of the hypersensitive infant is the treatment with heat at 110 ° C ( special milk), which determines the definitive denaturation of the immunogenetic molecules, preventing any allergic complication even in this type of disorder.
- pages 170-173