In the "last episode we saw what diverticula are, why they form in the colon and under what conditions they can become inflamed. Today we will investigate which disorders can determine diverticulitis and how" it can be diagnosed and treated. Before proceeding, however, a brief review is useful.
The diverticula of the colon are small protrusions, similar to pockets or sacs, present along the walls of the intestine. The presence of these diverticula is indicated by the medical term diverticulosis and generally does not create significant disturbances to the patient. The appearance of a diverticulum is essentially due to the addition of two factors: on the one hand we have the weakening of the muscular layer present in the colon walls, on the other hand an increase in pressure coming from the inside. Due to this pressure increase, often linked to constipation problems, there is a collapse of the intestinal wall in the points of least resistance, so the mucosa is extroverted, originating the diverticulum. Diverticula can form in various parts of the digestive tract, but are more common in the last part of the intestine. Therefore, in these episodes, we are focusing exclusively on the diverticula of the colon.In itself, diverticulosis would not be particularly problematic, except that under certain conditions the diverticula can become inflamed. In such circumstances, we no longer speak of diverticulosis but of diverticulitis, a pathology that can have serious consequences for the patient. Diverticulitis is an infectious disease; in fact, the inflammatory process is linked to the excessive proliferation of certain bacteria, which find an ideal habitat in the fecal material that stagnates in the diverticula.
Precisely because the presence of diverticula is often asymptomatic, in many cases their discovery is completely causal. For example, the doctor may notice diverticula thanks to a radiological examination of the digestive system or during a colonoscopy performed for other reasons. On the other hand, when the diverticula become inflamed, it is the patient himself who realizes that something in the intestine is not working properly. In fact, diverticulitis is accompanied by several symptoms. The most common is undoubtedly abdominal pain, which appears suddenly and often tends to concentrate in the left and lower abdomen, where the sigma is located. I remind you that the sigma is one of the last stretches of the intestine, and due to of the greatest pressure represents a preferential site for the formation of diverticula. In addition to abdominal pain, diverticulitis can be associated with nausea, vomiting, fever, bloating, bloating, and alternating constipation-diarrhea. In many cases, these symptoms are confused with those of other intestinal disorders and, for this reason, they are most often underestimated by the patient.
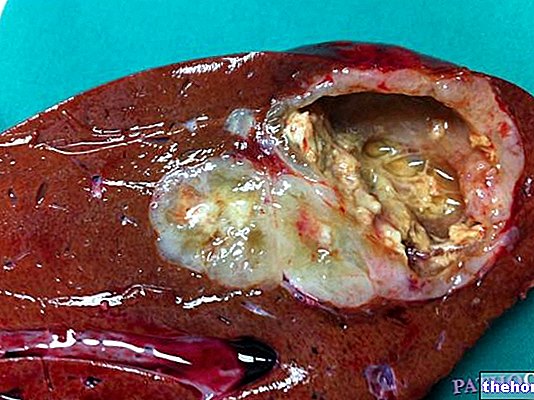
Too bad, however, that neglecting the inflammation of the diverticula can be very risky. In turn, diverticulitis can lead to various complications, ranging from the extension of the inflammatory process to nearby structures to perforation of the intestinal wall. Let's see them briefly in detail. First of all, if the infection that causes diverticulitis worsens, it can cause the formation of local abscesses, which are small pockets filled with pus. If these sacs burst, they can give rise to fistulas, which are canaliculi that connect the affected part of the colon and a nearby organ, such as the bladder or skin. Repeated episodes of diverticulitis can lead to the appearance of other complications, such as occlusion of the intestinal lumen; this obstruction is linked to the growth of inflammatory, scar-like tissue. The lesions can also bleed, and this bleeding is often evident in the presence of blood in the stool. In severe but fortunately rare cases, the rupture of an inflamed diverticulum can develop into peritonitis. In fact, bacteria can escape from the intestinal opening and through the peritoneum can spread to other organs and to the whole organism causing the so-called sepsis, a generalized infection that is often lethal.
As for the diagnosis, the presence of diverticula can be evidenced by various instrumental examinations. These include the so-called double-contrast barium enema and computed tomography that we all know as CT. Colonoscopy can also highlight the presence of diverticulitis and any lesions of the intestinal wall. However, it should be noted that colonoscopy and barium enema are not recommended in the acute phase of diverticulitis, due to the risk of colonic perforation. In these cases, it is preferable to resort to CT, which is essential to exclude other pathologies, assess the degree of severity of the disease and guide therapeutic management.
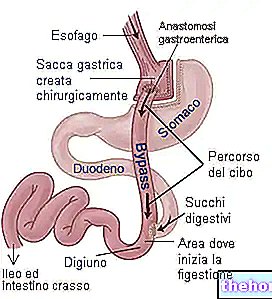
Generally, in the face of diverticulitis, the doctor recommends drug therapy supported by a diet free of irritants and initially low in fiber. Given the infectious nature of the disease, the most commonly used medicines are antibiotics. In addition, drugs that help to control pain and colic spasm, therefore painkillers and antispasmodics, may also be indicated. Only in some selected cases, is it necessary to resort to surgery. For example, surgery can be considered when episodes of diverticulitis are recurrent and if dangerous complications have arisen. Depending on the case, the intervention may include the removal of the diseased colon, with the rejoining of the two remaining healthy parts, the drainage of an abscess or a temporary colostomy. In the latter case, the colon is made to flow outwards, through the abdominal wall, in order to divert the intestinal contents to allow time for the diseased area to heal without contamination of the stool. second surgery to restore the normal intestinal passage.
Preventing colon diverticula and their complications means adopting correct behavioral rules, both at the table and in everyday life. To keep the intestine as regular as possible, a balanced diet and a good intake of fiber is recommended, accompanied by an abundant intake of water. Although a high-fiber diet is recommended, don't overdo it. In particular, a classic dietary rule provides for the limitation of all those vegetables or fruits that leave a large component of fiber in the intestine, such as those rich in seeds. Therefore, foods such as legumes, tomatoes, strawberries, kiwis, cucumbers, grapes, figs and dried fruit should be limited. Artichokes and fennel can also complicate the inflammation condition. All these recommendations would be justified by the fact that the excess of seeds and fibers tends to settle in the diverticula, favoring bacterial growth and their inflammation. However, not all doctors agree that this dietary rule is useful. Fibers aside, it is. It is also important to follow a diet free of irritants, such as spicy spices, alcohol, tea, coffee, carbonated drinks, chocolate and particularly fatty foods. These foods could in fact promote inflammation of the diverticula. Finally, it is certainly important to devote time to regular physical activity: long walks are also good, as movement helps to keep the muscles of the abdominal wall toned and also improves intestinal motility.