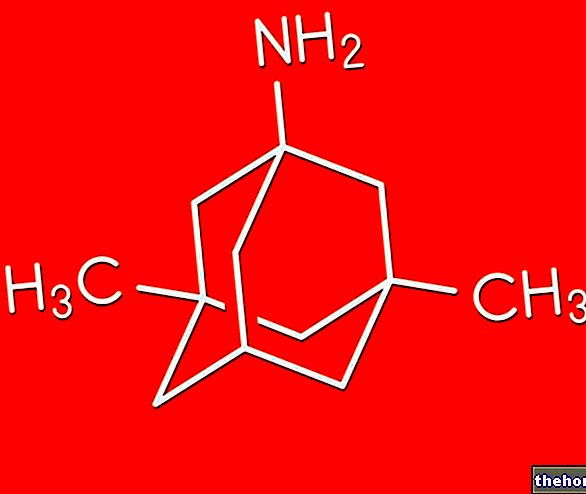
Active ingredients: Gestodene, Ethinylestradiol
GINODEN 0.075 mg + 0.03 mg coated tablets
Why is Ginoden used? What is it for?
Important things to know about combined hormonal contraceptives (COCs):
- They are one of the most reliable reversible methods of contraception when used correctly
- They slightly increase the risk of having blood clots in the veins and arteries, especially during the first year of taking or when restarting a combined hormonal contraceptive after a break of 4 or more weeks
- Take care and see your doctor if you think you have symptoms of a blood clot (see section "Blood clots")
PHARMACOTHERAPEUTIC CATEGORY
Progestogens and estrogens, fixed combinations.
THERAPEUTIC INDICATIONS
Prevention of conception.
Contraindications When Ginoden should not be used
Hypersensitivity to the active substances or to any of the excipients.
Do not use Ginoden if you have any of the conditions listed below. If you have any of the conditions listed below, please contact your doctor. Your doctor will discuss with you other birth control methods that may be more suitable for you.
- if you have (or have ever had) a blood clot in a blood vessel of the leg (deep vein thrombosis, DVT), lung (pulmonary embolism, PE) or other organs;
- if you know you have a disorder that affects blood clotting, such as protein C deficiency, protein S deficiency, antithrombin-III deficiency, factor V Leiden or antiphospholipid antibodies;
- if you are due to have an "operation or if you are going to lie down for a long time (see section" Blood clots ");
- if you have ever had a heart attack or stroke;
- if you have (or have ever had) angina pectoris (a condition that causes severe chest pain and may be a first sign of a heart attack) or transient ischemic attack (TIA - temporary stroke symptoms);
- if you have any of the following diseases, which could increase the risk of blood clots in the arteries:
- severe diabetes with blood vessel damage
- very high blood pressure
- very high level of fat (cholesterol or triglycerides) in the blood
- a disease known as hyperhomocysteinemia
- if you have (or have ever had) a type of migraine called 'migraine with aura';
- Jaundice (yellowing of the skin) or severe liver disease, present or past.
- Tumor of the breast or genital organs, present or previous.
- Benign or malignant liver tumor, present or previous.
- Vaginal bleeding of unknown origin.
- Known or suspected pregnancy.
- association with Ritonavir;
- ophthalmic pathology of vascular origin;
If any of these conditions appear for the first time while using the product, stop taking it immediately and consult your doctor. In the meantime, use non-hormonal methods of contraception. See also "General Notes".
Special populations
Pediatric population
The safety and efficacy of Ginoden in children and adolescents below 18 years of age have not been established. There are no data available.
Hepatic impairment
Do not take Ginoden if you have liver disease. See "Contraindications" and "Precautions for use".
Renal impairment
Ginoden has not been specifically studied in patients with impaired renal function.
Precautions for use What you need to know before taking Ginoden
General notes
Before you start using Ginoden you should read the information on blood clots in the section "Blood clots"). It is particularly important to read the symptoms of a blood clot (see section "Blood clots").
When should you see a doctor?
Contact a doctor urgently
- if you notice possible signs of a blood clot which may indicate that you are suffering from a blood clot in the leg (deep vein thrombosis), a blood clot in the lung (pulmonary embolism), a heart attack or a stroke (see section below " Blood clot (thrombosis) "). For a description of the symptoms of these serious side effects go to the section "How to recognize a blood clot".
This leaflet describes some situations in which it is necessary to stop taking the product or in which a reduction in the efficacy of the product itself may occur. In such situations you should not have sexual intercourse or you should take extra non-hormonal contraceptive precautions such as the use of condoms or other barrier methods. Do not use rhythm and basal temperature methods, which can be unreliable, as the pill alters the normal changes in temperature and cervical mucus that occur during the menstrual cycle.
This leaflet describes some situations in which it is necessary to stop taking the product or in which a reduction in the efficacy of the product itself may occur. In such situations you should not have sexual intercourse or you should take extra non-hormonal contraceptive precautions such as the use of condoms or other barrier methods. Do not use rhythm and basal temperature methods, which can be unreliable, as the pill alters the normal changes in temperature and cervical mucus that occur during the menstrual cycle.
Before starting or resuming taking the pill it is advisable to make a thorough medical examination
Furthermore, it is advisable to carry out periodic control visits, at least once a year, during the use of the product.
The frequency and type of visit will be established by the doctor and aimed in particular at blood pressure control, an examination of the breasts, abdomen and general gynecology including a Pap test and relative blood tests.
Like all contraceptive pills, Ginoden does not protect against HIV infection (AIDS) or any other sexually transmitted disease.
Ginoden is prescribed for personal use and must not be available to several people at the same time.
Precautions
In the presence of any of the conditions listed below, the use of the combined pill may require close medical supervision. It is therefore necessary to warn your doctor of any of the above conditions before starting to use Ginoden. Your doctor may recommend a completely different (non-hormonal) method of contraception.
Tell your doctor if any of the following apply to you.
If this condition appears or worsens while you are using Ginoden you should tell your doctor.
- Smoke;
- diabetes;
- overweight;
- hypertension;
- heart valve defects or certain heart rhythm disturbances;
- superficial phlebitis (venous inflammation);
- varicose veins;
- a history of thrombosis, heart attack or stroke in immediate family members;
- migraine;
- depression;
- epilepsy (see "Interactions");
- high levels of cholesterol and triglycerides (fats) in the blood, present or in the past, even in close family members;
- breast lumps;
- history of breast cancer in close relatives;
- liver or gallbladder disease;
- porphyria;
- present or previous chloasma (yellowish-brown pigmented patches on the skin, particularly on the face). In this case, avoid prolonged exposure to the sun or ultraviolet rays;
- previous herpes gestationis;
- some pathological conditions characterized by resistance to Activated Protein C, hyperhomocysteinemia, antithrombin III deficiency, protein C deficiency, protein S deficiency, antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant), which predispose to the onset of venous or arterial thrombosis;
- Sydenham's chorea (central nervous system disorder);
- hearing loss from otosclerosis.
- if you have hereditary angioedema, products containing estrogen may induce or aggravate the symptoms of angioedema. If you notice symptoms of angioedema such as swelling of the face, tongue and / or pharynx and / or difficulty swallowing or hives with difficulty in breathing, notify your doctor immediately.
- if you have Crohn's disease or ulcerative colitis (chronic inflammatory bowel disease);
- if you have systemic lupus erythematosus (SLE, a disease that affects the natural defense system);
- if you have haemolytic uremic syndrome (HUS, a blood clotting disorder causing kidney failure);
- if you have sickle cell anemia (an inherited disease of the red blood cells);
- if you have high levels of fat in the blood (hypertriglyceridaemia) or a "positive family history of this condition." Hypertriglyceridaemia has been associated with an increased risk of developing pancreatitis (inflammation of the pancreas);
- if you are due to have an "operation or if you are going to lie down for a long time (see section" Blood clots ");
- if you have just given birth, your risk of developing blood clots is higher. Ask your doctor how soon after having a baby you can start taking Ginoden;
- if you have "inflammation of the veins under the skin (superficial thrombophlebitis);
- if you have varicose veins.
In case of first appearance, recurrence or worsening of any of the above conditions while using the pill, consult your doctor.
Hypericum perforatum preparations should not be taken concomitantly with medicinal products containing oral contraceptives, digoxin, theophylline, carbamazepine, phenobarbital, phenytoin due to the risk of decreased plasma levels and decreased therapeutic efficacy of oral contraceptives, digoxin, theophylline, carbamazepine, phenobarbital, phenytoin (see section Interactions).
Interactions Which drugs or foods can modify the effect of Ginoden
Tell your doctor or pharmacist if you have recently taken any other medicines, even those without a prescription.
Some medications can affect the blood levels of Ginoden and prevent the pill from working effectively. These include:
- primidone, phenytoin, barbiturates, carbamazepine, oxycarbamazepine, topiramate, felbamate) (used to treat epilepsy),
- rifampicin (used to treat tuberculosis) and rifabutin,)
- protease inhibitors and non-nucleoside reverse transcriptase inhibitors, e.g. ritonavir and nevirapine (used to treat infections such as HIV and hepatitis C);
- griseofulvin (used to treat other infections), azole antifungals, such as itraconazole, voriconazole, fluconazole (used to treat fungal infections)
- macrolide antibiotics such as clarithromycin, erythromycin (used to treat bacterial infections)
- calcium channel blockers such as verapamil and diltizem (used to treat certain heart conditions and high blood pressure)
- etoricoxib (arthritis, osteoarthritis)
- modafinil and flunarizine.
Other antiepileptic drugs (oxcarbamazepine, topiramate, felbamate) are also likely to reduce the effectiveness of the pill. Ginoden can interfere with the mechanism of action of other medicines, for example:
- medicines containing cyclosporine
- l "anti-epileptic lamotrogine - melatonin - midazolam
- theophylline
- tizanidine
- omeprazole
Preparations based on hypericum perforatum should not be administered simultaneously with oral contraceptives, as this could lead to a loss of contraceptive efficacy. Unwanted pregnancies and resumption of the menstrual cycle have been reported. This is due to the induction of enzymes responsible for the metabolism of drugs from the preparations based on hypericum perforatum.
The induction effect may persist for at least 2 weeks after stopping treatment with hypericum perforatum products. Always inform the prescribing doctor about any medications you are already taking, and also inform any other doctors or dentists prescribing other medications that you are using Ginoden, so they can determine if and for how long it is needed. use additional contraceptive methods.
Using the pill can affect the results of some blood tests, but these changes are usually within the normal range. Therefore it is advisable to inform the doctor who requested the tests that you are taking the pill. Ginoden should not be taken with grapefruit juice.
Warnings It is important to know that:
BLOOD CLOTS
Using a combined hormonal contraceptive such as Ginoden increases your risk of developing a blood clot compared with not using one. In rare cases, a blood clot can block blood vessels and cause serious problems. Blood clots can develop.
- in veins (called "venous thrombosis", "venous thromboembolism" or VTE)
- in the arteries (referred to as 'arterial thrombosis', 'arterial thromboembolism' or ATE).
Recovery from blood clots is not always complete. Rarely, long-lasting severe effects can occur or, very rarely, they can be fatal.
It is important to remember that the overall risk of a harmful blood clot associated with Ginoden is low.
HOW TO RECOGNIZE A BLOOD CLOT
See a doctor immediately if you notice any of the following signs or symptoms.
- swelling of one leg or along a vein in the leg or foot, especially when accompanied by:
- pain or tenderness in the leg which may only be felt when standing or walking
- increased sensation of heat in the affected leg
- change in color of the skin on the leg, such as turning pale, red or blue
- sudden and unexplained shortness of breath or rapid breathing;
- sudden cough with no obvious cause, possibly causing blood to be emitted;
- sharp chest pain which may increase with deep breathing;
- severe light headedness or dizziness;
- rapid or irregular heartbeat;
- severe pain in the stomach
- immediate loss of vision or
- painless blurring of vision which can progress to loss of vision
- chest pain, discomfort, feeling of pressure or heaviness
- sensation of squeezing or fullness in the chest, arm or below the breastbone;
- feeling of fullness, indigestion or choking;
- upper body discomfort radiating to the back, jaw, throat, arms and stomach;
- sweating, nausea, vomiting or dizziness;
- extreme weakness, anxiety, or shortness of breath;
- rapid or irregular heartbeats
- sudden numbness or weakness of the face, arm or leg, especially on one side of the body;
- sudden confusion, difficulty speaking or understanding;
- sudden difficulty seeing in one or both eyes;
- sudden difficulty walking, dizziness, loss of balance or coordination;
- sudden, severe or prolonged migraine with no known cause;
- loss of consciousness or fainting with or without seizures.
- swelling and pale blue discoloration of one extremity;
- severe stomach pain (acute abdomen)
BLOOD CLOTS IN A VEIN
What can happen if a blood clot forms in a vein?
- The use of combined hormonal contraceptives has been linked to an increased risk of blood clots forming in the veins (venous thrombosis). However, these side effects are rare. In most cases they occur in the first year of using a combined hormonal contraceptive.
- If a blood clot forms in a vein in the leg or foot, it can cause a deep vein thrombosis (DVT).
- If a blood clot travels from the leg and lodges in the lung, it can cause a "pulmonary embolism."
- Very rarely, a clot can form in another organ such as the eye (retinal vein thrombosis).
When is the risk of developing a blood clot in a vein highest?
The risk of developing a blood clot in a vein is highest during the first year of taking a combined hormonal contraceptive for the first time. The risk may be even higher if you restart taking a combined hormonal contraceptive (the same drug or a different drug) after a break of 4 or more weeks.
After the first year, the risk is reduced but is always slightly higher than if you were not using a combined hormonal contraceptive.
When you stop taking Ginoden, the risk of developing a blood clot returns to normal within a few weeks.
What is the risk of developing a blood clot?
The risk depends on your natural risk of VTE and the type of combined hormonal contraceptive you are taking.
The overall risk of developing a blood clot in the leg or lung (DVT or PE) with Ginoden is low.
- Out of 10,000 women who are not using any combined hormonal contraceptive and who are not pregnant, about 2 will develop a blood clot in a year.
- Out of 10,000 women who are using a combined hormonal contraceptive that contains levonorgestrel, norethisterone or norgestimate, about 5-7 will develop a blood clot in a year.
- Out of 10,000 women who are using a combined hormonal contraceptive that contains gestodene, such as Ginoden, about 9-12 will develop a blood clot in a year.
- The risk of a blood clot forming depends on your medical history (see under "Factors that increase the risk of a blood clot forming").
Factors that increase the risk of developing a blood clot in a vein
The risk of developing a blood clot with Ginoden is low but some conditions cause it to increase. Its risk is greater:
- if you are severely overweight (body mass index or BMI above 30 kg / m2);
- if a member of your immediate family has had a blood clot in the leg, lung or other organ at a young age (less than about 50 years). In this case you could have an inherited blood clotting disorder;
- if you are going to have an operation or if you have to lie down for a long time because of an injury or illness or if you have a leg in a cast. You may need to stop taking Ginoden a few weeks before the surgery or in the period in which you are less mobile. If you have to stop taking Ginoden ask your doctor when you can start taking it again;
- as you get older (especially over the age of 35);
- if you gave birth less than a few weeks ago
The risk of developing a blood clot increases the more conditions you have of this type. Air travel (lasting> 4 hours) may temporarily increase the risk of a blood clot, especially if you have some of the other risk factors listed.
It is important that you tell your doctor if any of these apply to you, even if you are not sure. Your doctor may decide that Ginoden needs to be stopped.
If any of the above conditions change while you are using Ginoden, for example if a close relative has a thrombosis for no known reason or if you gain a lot of weight, contact your doctor.
BLOOD CLOTS IN AN ARTERY
What can happen if a blood clot forms in an "artery?"
Like blood clots in a vein, clots in an artery can cause serious problems, for example, they can cause a heart attack or stroke.
Factors that increase the risk of developing a blood clot in an artery
It is important to note that the risk of heart attack or stroke associated with the use of Ginoden is very low but can increase:
- with increasing age (over 35 years);
- if you smoke. When using a combined hormonal contraceptive like Ginoden you are advised to stop smoking. If you are unable to stop smoking and are over the age of 35, your doctor may advise you to use a different type of contraceptive;
- if you are overweight;
- if you have high blood pressure;
- if a member of your immediate family has had a heart attack or stroke at a young age (less than about 50 years). In this case, you may also be at high risk of having a heart attack or stroke;
- if you or a close relative have a high level of fat in the blood (cholesterol or triglycerides);
- if you suffer from migraines, especially migraines with aura;
- if you have any heart problems (valve defect, a heart rhythm disorder called atrial fibrillation);
- if you have diabetes.
If you have more than one of these conditions or if any of them are particularly severe, the risk of developing a blood clot may be even higher.
If any of the above conditions change while you are using Ginoden, for example if you start smoking, if a close relative has a thrombosis for no known reason or if you gain a lot of weight, contact your doctor.
Tumors
Breast cancer diagnoses are slightly more common in women who use the pill than in those of the same age who do not. The slight increase in the number of breast cancer diagnoses gradually disappears over the 10 years following discontinuation of treatment. It is not known if the difference is due to the pill.
This increase may be due to earlier diagnosis, as women are seen more frequently, the biological effect of the pill, or both. Breast cancer diagnosed in women taking the pill tends to be less clinically advanced than breast cancer. diagnosed in women who do not use it.
Benign liver tumors and even more rarely malignant liver tumors have been reported in women taking the Pill. Such tumors can cause internal bleeding. Consult your doctor immediately in case of severe pain in the abdomen.
Cancer of the neck of the uterus (cervix) has been reported to be more common in women who use the pill for a long time. genesis of tumors in general.
The aforementioned tumors can be life-threatening or fatal.
Pregnancy and breastfeeding
Ask your doctor or pharmacist for advice before taking any medicine.
Ginoden must not be used in known or suspected pregnancy.
Ginoden is not recommended while breastfeeding.
Effects on ability to drive and use machines
No effects on the ability to drive and use machines have been observed.
Important information about some of the ingredients
Ginoden contains lactose. If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicinal product.
Ginoden contains sucrose. If you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicinal product.
WHEN IS IT NECESSARY TO CONSULT THE DOCTOR?
Contact a doctor urgently
- if you notice possible signs of a blood clot which may indicate that you are suffering from a blood clot in the leg (deep vein thrombosis), a blood clot in the lung (pulmonary embolism), a heart attack or a stroke (see section below " Blood clot (thrombosis) ").
For a description of the symptoms of these serious side effects go to the section "How to recognize a blood clot".
Periodic checks
While using the pill, your doctor will ask you to come to periodic check-ups, usually every year.
See your doctor as soon as possible:
- if you observe any change in your state of health, particularly related to what is reported in this leaflet (see also "Contraindications" and "Precautions for" use ". Do not forget the references to close family members);
- if you feel a lump in your breast
- if other medications are to be used (see also "Interactions");
- if you are immobilized or have to undergo surgery (consult your doctor at least four weeks before);
- if you have severe and unusual vaginal bleeding;
- if you have missed tablets in the first week of use and have had sexual intercourse in the seven days prior to the forgetfulness;
- if you do not have a period for two consecutive cycles or if you suspect a pregnancy, do not start a new pack without your doctor's permission.
Stop taking the tablets and consult your doctor immediately if you notice possible signs of thrombosis:
- cough that starts suddenly;
- severe pain in the chest that may radiate to the left arm;
- sudden shortness of breath;
- unusual, severe, prolonged headache or migraine attack;
- partial or total loss of vision or double vision;
- slurred speech or inability to speak;
- sudden changes in hearing, smell and taste;
- feeling dizzy or faint;
- weakness or numbness of any part of the body;
- severe abdominal pain;
- severe pain or swelling in one leg.
The above situations and symptoms are illustrated and explained in more detail in other sections of this leaflet.
Dose, Method and Time of Administration How to use Ginoden: Posology
Ginoden pack contains 21 tablets, all marked with the day of the week on which each should be taken. Take the tablet at approximately the same time every day, if necessary with a little water. Follow the direction of the arrows until all 21 tablets have been used up. Do not take pills within the next 7 days, during which they should appear menstruation (withdrawal bleeding), which usually begins 2-3 days after taking the last Ginoden tablet. Start the new pack on the eighth day, even if your period has not yet finished. By doing so, the new package will always be started on the same day of the week and the withdrawal bleeding will always occur on approximately the same days of the week, every month.
COCs, when taken correctly, have a 1% failure rate per year. The failure rate increases when pills are forgotten or not taken correctly.
Beginning of the first pack
- No hormonal contraceptive in the previous month.
Start taking Ginoden on the first day of your period, which is the first day of your period, taking the tablet marked with that day of the week. For example, if your period starts on a Friday, take the pill marked with Friday. order indicated by arrows. It can also start between the second and fifth day of the cycle, but in this case an additional contraceptive method (barrier method) must be used for the first seven days of tablet-taking in the first cycle.
- Switching from another "combined type" pill from a vaginal ring, or a patch.
You can start taking Ginoden the day after the last pill of the previous contraceptive (ie without observing any interval). If your previous contraceptive pack also contains inactive tablets, you can take Ginoden the day after the last active tablet (in case if in doubt, ask your doctor). It can also be started later, but never later than the day after the pill-free interval (or the day after the last inactive tablet) of the previous contraceptive. If you have used a vaginal ring or patch, you should start using Ginoden preferably on the day of removal, the last ring or patch of a cycle, or at the latest when your next application should have been. If you follow these instructions, do not. it is necessary to use an additional method of contraception.
- Changing from a progestogen-only pill (minipill).
You can stop taking the minipill on any day and start taking Ginoden the next day at the same time. However, for the first seven days of taking the tablets, use an additional method of contraception (barrier method) when having intercourse.
- Changing from an injection or implantation contraceptive or a progestogen-releasing intrauterine system (IUS).
Start using Ginoden on the day the next injection is due or the day the implant is removed. However, in the first seven days of taking the tablets use an additional contraceptive method (barrier method) when having intercourse. .
- After giving birth.
The start of the pill after childbirth must be determined by the doctor. He will decide whether to start the treatment in the period between the 21st and the 28th day, or later. In the latter case it is advisable to use an additional barrier method in the first 7 days of taking the tablets. However, if you have had sexual intercourse in the meantime, you must rule out pregnancy or wait for your first menstruation before starting the pill. If you are breastfeeding and want to take Ginoden, talk to your doctor first.
- After a spontaneous or induced abortion.
Follow your doctor's prescription.
Termination of employment
You can stop using Ginoden at any time. If you do not want to become pregnant, consult your doctor about other methods of birth control.
If you want to stop using Ginoden because you want to be pregnant, talk to your doctor. In this case it is generally advisable to wait until your period is regular again before attempting to conceive.
WHAT TO DO IF ...
you forget to take your tablets
- If less than 12 hours have passed since the time of usual intake, the reliability of the pill is preserved. Take the forgotten tablet as soon as you remember and continue as usual.
- If more than 12 hours have passed since the time of usual intake, the reliability of the pill may be reduced. The greater the number of consecutively forgotten tablets, the greater the risk of the contraceptive effect being reduced. The risk of pregnancy is particularly high if pills are forgotten at the beginning and at the end of the pack. Follow the instructions below (see also the diagram below).
More than one tablet forgotten in one pack
Consult your doctor.
One tablet forgotten in the first week
Take the tablet as soon as you remember (even if that means taking two tablets at the same time) and continue as usual. Use additional contraceptive methods (barrier method) for the next 7 days.
If you have had sexual intercourse in the week preceding the forgetfulness, it is possible that you are pregnant. Inform your doctor immediately.
One tablet forgotten in the second week
Take the forgotten tablet as soon as you remember (even if that means taking two tablets at the same time) and continue as usual. The reliability of the pill is preserved. No additional contraceptive precautions need to be taken.
One tablet forgotten in the third week
One of the following alternatives may be chosen, without the need for additional contraceptive precautions.
1. Take the forgotten tablet as soon as you remember (even if that means taking two tablets at the same time) and continue as usual. Start the new pack as soon as the current one is finished, with no gap between the two packs. Withdrawal bleeding may not occur until the second pack is finished, but intermenstrual bleeding (spotting) may occur during the days of intake.
or
2. Discontinue the tablets from the current pack, observe an interval of 7 days or less (also count the day of the missed pill) and continue with a new pack. If you choose this alternative, you can always start the new pack on the same day of the week on which you usually start.
If you forget to take one or more tablets and do not have a period in the first pill-free interval, you may have become pregnant. Consult your doctor before starting the new pack.
In case of gastrointestinal disturbances (e.g. vomiting and / or diarrhea)
If you experience vomiting or severe diarrhea within 3-4 hours of taking Ginoden, it is possible that the active substance has not been completely absorbed. It is as if the tablet had been forgotten. Therefore, follow the instructions given in case of missed tablets.
Delayed menstruation: what you need to know
Although not recommended, it is possible to delay your period by continuing with a new pack of Ginoden without observing the 7-day interval. You may experience breakthrough bleeding or spotting while using this second pack. Continue with the next pack after the usual 7-day interval.
It is therefore necessary to ask your doctor for advice before deciding to delay menstruation.
Changing the start day of your period: what you need to know
If you take the tablets according to the instructions, your period will start on about the same day of the week. If you have to change this day, you can shorten (never lengthen!) The normal break between two consecutive packs. For example, if your period is generally start on Friday and you want them to start on Tuesday (3 days earlier), you will have to start the next pack 3 days in advance. If you make the break between two cycles too short (e.g. 3 days or less), you can you do not have a period during this period, in which case you may have breakthrough bleeding or spotting during the next course of treatment.
You should contact your doctor if you are unsure how to proceed.
In case of unexpected bleeding
With all oral contraceptives, vaginal bleeding can occur in the first few months of taking it between menstruation. Normally, irregular bleeding disappears once the body gets used to the pill (usually after about 3 cycles of assumption). It is always advisable to consult your doctor, but especially if these bleeding persist, become intense or recur at intervals.
In case of missed menstruation
If all the tablets have been taken correctly, no vomiting has occurred or other medications have been taken, it is very unlikely that you are pregnant. Continue using the product as usual.
If your period does not occur twice in a row, it is possible that you are pregnant. Consult your doctor immediately. Do not start the new pack until your doctor has ruled out pregnancy.
Overdose What to do if you have taken too much Ginoden
There have been no reports of serious side effects when taking several tablets at the same time. In this case, nausea, vomiting or vaginal bleeding may occur.
In case of accidental ingestion / intake of an overdose of Ginoden, notify your doctor immediately or go to the nearest hospital.
If you have any further questions on the use of Ginoden, ask your doctor or pharmacist.
Side Effects What are the side effects of Ginoden
Like all medicines, Ginoden can cause side effects, although not everybody gets them. If you get any side effects, especially if they are severe or persistent, or if there is any change in your health that you think might be due to Ginoden, please tell your doctor.
An increased risk of developing blood clots in the veins (venous thromboembolism (VTE)) or blood clots in the arteries (arterial thromboembolism (ATE)) is present in all women taking combined hormonal contraceptives. For more detailed information on the different risks arising from "taking combined hormonal contraceptives, see section" Special warnings ".
Serious side effects
Serious adverse reactions associated with the use of the pill, and related symptoms, are described in the section "Precautions for use", "Blood clots" and "Cancers". For more information read these paragraphs and consult your doctor immediately.
Other side effects
The following side effects have been reported in women using the Pill:
- breast tension, pain and discharge;
- headache, migraine;
- changes in sexual desire, depressed mood;
- contact lens intolerance;
- nausea, vomiting and feeling unwell;
- changes in vaginal secretions;
- skin reactions;
- fluid retention;
- changes in body weight;
- hypersensitivity reactions;
- oligomenorrhea, amenorrhea;
- intermenstrual bleeding; or harmful blood clots in a vein or artery, for example:
- in one leg
- in one foot (DVT)
- in a lung (EP)
- heart attack
- stroke or mini-stroke
- temporary stroke-like symptoms, known as a transient ischemic attack (TIA)
- blood clots in the liver, stomach / intestines, kidneys or eye.
The chance of developing a blood clot may be higher if you have any other conditions that increase this risk (see section "Special warnings" for more information on conditions that increase the risk of blood clots and the symptoms of a blood clot)
In women with hereditary angioedema, exogenous estrogens can induce or aggravate the symptoms of angioedema.
Compliance with the instructions contained in this leaflet reduces the risk of undesirable effects.
Presentation of undesirable effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. Undesirable effects can also be reported directly through the national reporting system at "https://www.aifa.gov.it/content/segnalazioni-reazioni-avverse". By reporting side effects you can help provide more information on the safety of this medicine.
Expiry and Retention
Expiry: see the expiry date printed on the package.
The expiry date refers to the product in intact packaging, correctly stored.
CAUTION: DO NOT USE THE MEDICINAL PRODUCT AFTER THE EXPIRY DATE INDICATED ON THE PACKAGE.
STORAGE PRECAUTIONS
Do not store above 25 ° C. Store in the original package to protect the medicine from light.
Store all medications properly.
Do not use the product if you notice, for example, a change in color or crumbling of the tablet, or in the presence of any other visible sign of deterioration.
Medicines should not be disposed of via wastewater or household waste.
Ask your pharmacist how to throw away medicines you no longer use. This will help protect the environment.
Keep this medicine out of the sight and reach of children.
COMPOSITION
Each coated tablet contains:
Active principles:
gestodene 0.075 mg ethinyl estradiol 0.03 mg.
Excipients:
Lactose monohydrate, corn starch, povidone 25, sodium calcium edetate, magnesium stearate, sucrose, povidone 90, macrogol 6,000, calcium carbonate, talc, ethylene glycol ester of montanic acid (E wax).
PHARMACEUTICAL FORM AND CONTENT
Coated tablets for oral use.
The product is packaged in calendar blisters containing 21 coated tablets.
Source Package Leaflet: AIFA (Italian Medicines Agency). Content published in January 2016. The information present may not be up-to-date.
To have access to the most up-to-date version, it is advisable to access the AIFA (Italian Medicines Agency) website. Disclaimer and useful information.
01.0 NAME OF THE MEDICINAL PRODUCT
GINODEN 0.075 MG + 0.03 MG COATED TABLETS
02.0 QUALITATIVE AND QUANTITATIVE COMPOSITION
Each tablet contains 0.075 mg of gestodene and 0.03 mg of ethinylestradiol.
Excipients with known effects: lactose, sucrose.
For the full list of excipients, see section 6.1.
03.0 PHARMACEUTICAL FORM
Coated tablets.
04.0 CLINICAL INFORMATION
04.1 Therapeutic indications
Prevention of conception.
The decision to prescribe Ginoden must take into account the individual woman's current risk factors, particularly those related to venous thromboembolism (VTE) and the comparison between the risk of VTE associated with Ginoden and that associated with other combined hormonal contraceptives (COCs). (see sections 4.3 and 4.4).
04.2 Posology and method of administration
Method of administration
Oral use
Method of recruitment
COCs, when taken correctly, have a 1% failure rate per year. The failure rate increases when pills are forgotten or not taken correctly.
The tablets must be taken in the order indicated on the package, every day at the same time, if necessary with a little liquid; the dosage is one tablet per day for 21 consecutive days. Each subsequent pack should be started after a 7-day tablet-free interval during which a withdrawal bleed usually occurs. This usually starts 2-3 days after the last tablet and may not have finished before the next pack is started.
Methods of starting the treatment
No hormonal contraceptive treatment in the previous month
Taking the tablets should begin on the first day of the natural menstrual cycle (ie the first day of menstruation). It is also possible to start between the second and fifth day of the cycle but, in this case, during the first cycle it is also recommended to use a barrier method in the first seven days of taking the tablets.
Changing from another hormonal contraceptive (combined oral contraceptive, vaginal ring, patch)
The first tablet should preferably be taken on the day after the last active tablet of the previous contraceptive or at the latest on the day after the usual tablet-free break or the day after the last placebo tablet of the previous contraceptive. In case of changing from a vaginal ring or a patch, the woman should start taking Ginoden preferably on the day of the removal of the last ring or patch of a cycle of applications, or at the latest, when the next application would have been scheduled.
Changing from a progestogen-only contraceptive (minipill, injection, implant) or from a progestogen-releasing intrauterine system (IUS).
The woman can change at any time if she is coming from the minipill, and she must start taking Ginoden the next day. In the case of an implant, taking Ginoden must start on the same day the implant is removed or, in case of an injectable, on the day the next injection should be given. In all these cases the woman should also be advised to also use a supportive non-hormonal method of contraception for the first seven days of tablet-taking.
After a first trimester abortion
You can start immediately without the need for additional contraceptive measures.
After childbirth or second-trimester abortion
Since the immediate postpartum period is associated with an increased thromboembolic risk, the use of COCs should not commence earlier than the 21st-28th day after delivery or after a second trimester abortion. also use a supportive non-hormonal method of contraception during the first seven days of taking the tablets. However, if intercourse has occurred in the meantime, pregnancy must be ruled out or the first menstruation should be waited for before starting the COC.
For breastfeeding women see section 4.6.
Irregular intake
Contraceptive safety may decrease if tablets are forgotten, particularly if the forgotten occurs during the first few days of the treatment cycle.
If she is less than 12 hours late in taking any tablet, contraceptive protection is not reduced. The forgotten tablet should be taken as soon as she remembers and the following tablets should be taken at the usual pace.
If you are more than 12 hours late in taking any tablet, contraceptive protection is no longer ensured.
If you forget a tablet, the following principles apply:
1. Tablet-taking must never be interrupted for more than 7 days.
2. It takes 7 days of uninterrupted tablet-taking to achieve "adequate suppression of the hypothalamus-pituitary-ovarian axis."
Consequently, the following tips can be given in daily practice.
• First week
The last missed tablet should be taken as soon as the woman remembers, even if this means taking two tablets at the same time. The other tablets should be taken at the usual rhythm. In addition, a barrier method, such as a condom, should be used for the next 7 days. If intercourse took place in the previous week, the possibility of a pregnancy should be considered. The greater the number of missed tablets and the shorter the pill-free interval, the greater the risk of pregnancy.
• Second week
The last missed tablet should be taken as soon as the woman remembers, even if this means taking two tablets at the same time. The other tablets should be taken at the usual pace. It is not necessary to use any additional contraceptive methods, provided that, in the 7 days preceding the first missed tablet, the tablets have been taken correctly; however, if not, or if more than one forgotten tablet, the use of additional precautions for 7 days should be recommended.
• Third week
Given the imminence of the tablet-free interval, the risk of reduced contraceptive reliability is greater. However, modifying the pill-taking pattern can still prevent the reduction of contraceptive protection. By adopting either of the following two options there is therefore no need to use additional contraceptive methods as long as in the 7 days preceding the first missed tablet all tablets have been taken correctly. Otherwise it should be recommended to follow the first of the two options and also to use additional precautions for the next 7 days.
1. The last missed tablet should be taken as soon as the woman remembers, even if this means taking two tablets at the same time. The other tablets should be taken at the usual rhythm. The next pack should be started immediately after finishing the previous one, i.e. without observing the tablet-free interval between the two packs. In this case, withdrawal bleeding is unlikely to occur before the end of the second pack; however, spotting or breakthrough bleeding may occur while taking the tablets.
2. You may also be advised to stop taking tablets from the current pack. You should then observe a pill-free interval of up to 7 days, including those in which tablets have been missed, and then continue with a new one. packaging.
If tablets have been missed and no withdrawal bleeding occurs in the first regular tablet-free interval, the possibility of an existing pregnancy should be considered.
Recommendations in case of gastrointestinal disorders
In the case of severe gastrointestinal disorders, absorption may be impaired and additional contraceptive measures must be used.
If vomiting and / or diarrhea occurs within 3-4 hours of taking the tablet, absorption may not be complete. In this case, the recommendations outlined in the section "Irregular employment" should be considered if necessary. If the usual dosing schedule is not to be changed, one or more extra tablets should be taken from a new pack.
How to move your period from suspension
To delay a menstruation, the patient must continue to take the tablets by taking them from another pack of Ginoden without interruption. The delay can be extended according to the patient's wishes until the end of the second pack of tablets. During this prolonged intake, the patient can have breakthrough bleeding or spotting. Ginoden should be taken regularly after the usual 7 day break.
To shift the period to another day of the week than the expected day according to the patient's schedule, the treatment-free interval can be shortened to the desired days. The shorter the tablet-free interval, the greater the possibility of do not have a flow, but you may experience breakthrough bleeding or spotting while taking the next pack (such as when you want to delay your period).
Special populations
Pediatric population
The safety and efficacy of Ginoden in children and adolescents below 18 years of age have not been established. There are no data available.
Hepatic impairment
Ginoden is contraindicated in women with severe liver disease. See section 4.3.
Renal impairment
Ginoden has not been specifically studied in patients with impaired renal function.
04.3 Contraindications
Hypersensitivity to the active substances or to any of the excipients listed in section 6.1.
Combined hormonal contraceptives (COCs) should not be used in the following conditions. The product should be discontinued immediately, should any of the conditions appear for the first time while using the COC.
• Presence or risk of venous thromboembolism (VTE)
- Venous thromboembolism - VTE (with anticoagulants) or a history of VTE (eg deep vein thrombosis [DVT] or pulmonary embolism [PE])
- Known hereditary or acquired predisposition to venous thromboembolism, such as resistance to activated protein C (including factor V Leiden), antithrombin III deficiency, protein C deficiency, protein S deficiency
- Major surgery with prolonged immobilization (see section 4.4)
- High risk of venous thromboembolism due to the presence of multiple risk factors (see section 4.4)
• Presence or risk of arterial thromboembolism (ATE)
- Arterial thromboembolism - current or previous arterial thromboembolism (e.g. myocardial infarction) or prodromal conditions (e.g. angina pectoris)
- Cerebrovascular disease - current or previous stroke or prodromal conditions (e.g. transient ischaemic attack, TIA)
- Known hereditary or acquired predisposition to arterial thromboembolism, such as hyperhomocysteinaemia and antiphospholipid antibodies (anticardiolipin antibodies, lupus anticoagulant)
- History of migraine with focal neurological symptoms
- High risk of arterial thromboembolism due to the presence of multiple risk factors (see section 4.4) or the presence of a serious risk factor such as:
• diabetes mellitus with vascular symptoms
• severe hypertension
• severe dyslipoproteinemia
• severe liver disease, either current or past, until liver function values have returned to normal;
• liver tumors, current or past, benign or malignant;
• known or suspected malignant pathologies of the genital organs or breasts, if hormone-dependent;
• vaginal bleeding of an undetermined nature;
• known or suspected pregnancy;
• association with Ritonavir;
• ophthalmic pathology of vascular origin
04.4 Special warnings and appropriate precautions for use
If any of the conditions or risk factors mentioned below are present, the suitability of Ginoden should be discussed with the woman.
In the event of worsening or first appearance of any of these risk factors or conditions, the woman should contact her physician to determine whether the use of Ginoden should be discontinued.
Risk of venous thromboembolism (VTE)
The use of any combined hormonal contraceptive (COC) results in an increased risk of venous thromboembolism (VTE) compared with no use. Products that contain levonorgestrel, norgestimate or norethisterone are associated with a lower risk of VTE. The risk associated with others. products such as Ginoden can be doubled. The decision to use a product other than those associated with a lower risk of VTE should only be made after discussions with the woman to ensure that she understands the risk of VTE associated with Ginoden, the way where your current risk factors influence that risk and the fact that the risk of developing a VTE is highest in the first year of use. There is also some evidence that the risk increases when taking a COC is resumed after a break of 4 or more weeks.
About 2 in 10,000 women who do not use a CHC and who are not pregnant will develop a VTE over a period of one year. In a single woman, however, the risk can be much higher, depending on her underlying risk factors (see below).
It is estimated [1] that out of 10,000 women who use a CHC containing gestodene, between 9 and 12 will develop a VTE in one year; this compares with approximately 6 [2] women using a COC containing levonorgestrel.
[1] These incidences were estimated from the totality of epidemiological study data, using the relative risks of the different products compared to levonorgestrel-containing CHCs
[2] Median value of the range 5-7 per 10,000 women / year, based on a relative risk of approximately 2.3-3.6 of levonorgestrel-containing CHCs compared to non-use
In both cases, the number of VTEs per year is less than the number expected in pregnancy or in the postpartum period.
VTE can be fatal in 1-2% of cases.
Very rarely, thrombosis has been reported in CHC users in other blood vessels, e.g. hepatic, mesenteric, renal or retinal veins and arteries.
Risk factors for VTE
The risk of venous thromboembolic complications in CHC users may increase substantially if additional risk factors are present, especially if there are more than one risk factors (see table).
Ginoden is contraindicated if a woman has several risk factors that increase her risk of venous thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increased risk is greater than the sum of the individual factors; in this case her total risk of VTE should be considered. If the benefit-risk ratio is considered to be negative, a COC should not be prescribed (see section 4.3).
Table: Risk factors for VTE
There is no agreement on the possible role of varicose veins and superficial thrombophlebitis in the onset and progression of venous thrombosis.
The increased risk of thromboembolism in pregnancy, particularly the 6-week period of the puerperium, must be considered (for information on "Pregnancy and lactation" see section 4.6).
Symptoms of VTE (deep vein thrombosis and pulmonary embolism)
If symptoms of this type occur, women should seek immediate medical attention and inform them that they are taking a CHC.
Symptoms of deep vein thrombosis (DVT) can include:
- unilateral swelling of the leg and / or foot or along a vein in the leg;
- pain or tenderness in the leg which may only be felt when standing or walking;
- increased sensation of heat in the affected leg; skin on the leg that is red or discolored.
Symptoms of pulmonary embolism (PE) can include:
- sudden and unexplained onset of shortness of breath and rapid breathing;
- sudden cough which may be associated with hemoptysis;
- sharp pain in the chest;
- severe light headedness or dizziness;
- rapid or irregular heartbeat.
Some of these symptoms (such as "shortness of breath" and "cough") are non-specific and may be misinterpreted as more common or less serious events (eg respiratory tract infections).
Other signs of vascular occlusion may include: sudden pain, swelling or a pale blue discoloration of one "extremity.
If the occlusion takes place in the eye, symptoms can range from painless blurring of vision to loss of vision. Sometimes vision loss occurs almost immediately.
Risk of arterial thromboembolism (ATE)
Epidemiological studies have associated the use of CHCs with an increased risk of arterial thromboembolism (myocardial infarction) or of cerebrovascular accidents (eg transient ischemic attack, stroke). Arterial thromboembolic events can be fatal.
Risk factors of ATE
The risk of arterial thromboembolic complications or a cerebrovascular accident in CHC users increases in the presence of risk factors (see table). Ginoden is contraindicated if a woman has one serious risk factor or multiple risk factors for ATE that increase her risk of arterial thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors; in this case her total risk should be considered. If the benefit-risk balance is believed to be negative, a CHC should not be prescribed (see section 4.3).
Table: Risk factors of ATE
Symptoms of ATE
If symptoms of this type occur, women should contact a healthcare professional immediately and inform them that they are taking a CHC.
Symptoms of cerebrovascular accident can include:
- sudden numbness or weakness of the face, arm or leg, especially on one side of the body;
- sudden difficulty walking, dizziness, loss of balance or coordination;
- sudden confusion, difficulty in elocution or understanding;
- sudden difficulty seeing in one or both eyes;
- sudden, severe or prolonged migraine with no known cause;
- loss of consciousness or fainting with or without convulsions.
Temporary symptoms suggest it is a transient ischemic attack (TIA).
Symptoms of myocardial infarction (MI) can include:
- pain, discomfort, pressure, heaviness, sensation of squeezing or fullness in the chest, arm or below the breastbone;
- discomfort radiating to the back, jaw, throat, arms, stomach;
- feeling of fullness, indigestion or choking;
- sweating, nausea, vomiting or dizziness;
- extreme weakness, anxiety or shortness of breath;
- rapid or irregular heartbeats.
Medical examinations / visits
Before initiating or resuming use of Ginoden, a complete medical history (including family history) should be taken and pregnancy should be ruled out. Blood pressure should be measured and a clinical examination, guided by contraindications, should be performed (see section 4.3 ) and warnings (see section 4.4). It is important to draw a woman's attention to information relating to venous or arterial thrombosis, including the risk associated with Ginoden compared to other CHCs, symptoms of VTE and ATE, known risk factors and what to do in case of suspected thrombosis.
The woman should also be advised of the need to read the package leaflet carefully and to follow its advice. The frequency and type of examinations should be based on established guidelines and should be adapted to the individual woman.
Women should be advised that hormonal contraceptives do not protect against HIV infections (AIDS) and other sexually transmitted diseases.
Tumors
Carcinoma of the reproductive organs and breast
In some epidemiological studies an increased risk of cervical cancer has been reported in women on long-term treatment with COCs; however, there is still no consensus on the extent to which this finding is attributable to confounding effects due to sexual behavior and other factors such as human papilloma virus (HPV).
A meta-analysis of 54 epidemiological studies found that women currently using COCs have a slightly increased relative risk (RR = 1.24) of having breast cancer diagnosed and that the excess risk gradually disappears over the course of the of the 10 years following the interruption of treatment. Since breast cancer is rare in women under the age of 40, the extra number of breast cancers diagnosed in women taking or recently taking a combined oral contraceptive is low compared to the risk of breast cancer. it runs over a woman's entire life. These studies provide no evidence of this causal relationship. The observed increased risk may be due to an earlier diagnosis of breast cancer in women taking COCs, the biological effects of COCs. or a combination of both factors Breast cancer diagnosed in oral contraceptive users tends to be less clinically advanced than that diagnosed in women who have never used an oral contraceptive.
Hepatic neoplasia
Benign liver tumors and, even more rarely, malignant liver tumors have been reported rarely in women taking COCs. In isolated cases, these tumors have resulted in life-threatening intra-abdominal haemorrhage. If a woman taking a combined oral contraceptive develops severe upper abdominal pain, liver enlargement, or signs suggestive of intra-abdominal haemorrhage, the possibility of a liver tumor which may be dangerous should be considered when making the diagnosis. for life or be fatal.
Other conditions
Liver function
Acute or chronic disturbances of liver function may require discontinuation of COC treatment until markers of liver function have returned to normal. Return of cholestatic jaundice already occurring in pregnancy or during previous sex steroid treatment requires treatment. discontinuation of the combined oral contraceptive.
Eye injuries
Cases of retinal thrombosis have been reported during the use of COCs. If there is unexplained partial or complete loss of vision, the onset of proptosis or diplopia, papilledema or vascular lesions of the retina, use of the contraceptive Combined oral therapy should be discontinued and cause should be evaluated immediately.
Headache
The appearance or exacerbation of migraine or the development of headache with the characteristic being recurrent, persistent and severe, constitute situations which require discontinuation of the combined oral contraceptive and evaluation of the cause.
Effects on the metabolism of lipids and carbohydrates
Although COCs may affect peripheral insulin resistance and glucose tolerance, there is no evidence for the need for regimen adjustment in diabetic patients using COCs. diabetic patients must be carefully followed.
Women with hypertriglyceridaemia or a family history of this condition may have an increased risk of pancreatitis when taking COCs.
Folate levels
Serum folate levels may be decreased by combined oral contraceptive therapy. This may be of clinical importance if the woman becomes pregnant shortly after stopping the COC.
Fluid retention
COCs should be prescribed with caution to women whose medical conditions may be aggravated by fluid retention.
Blood pressure
The use of oral contraceptives is contraindicated in women with a history of hypertension or with diseases related to hypertension or kidney disease. Although a small rise in blood pressure has been reported in many women taking COCs, a clinically relevant increase is rare. A relationship between COC use and hypertension has not been established. However, if clinically significant hypertension occurs during the use of a COC, the physician should, as a precaution, stop taking the COC and treat the hypertension.
Pathologies of the intestine
Crohn's disease and ulcerative colitis have been reported in association with combined oral contraceptive use.
Disorders of the emotional sphere
Women who become significantly depressed while taking COCs should stop treatment and use an alternative method of contraception to determine if this symptom is drug-related. Women with a history of depression should be closely monitored and treatment should be discontinued if severe depression occurs.
Irregular bleeding
Irregular bleeding (spotting or breakthrough bleeding) may occur while taking any COC, especially in the first months of treatment. Therefore, the evaluation of any irregular vaginal bleeding is only meaningful after a settling phase of about 3 months. courses of treatment.
If irregular bleeding persists or occurs after previously regular cycles, a non-hormonal etiology should be considered and appropriate diagnostic measures, which may include curettage, should be implemented to rule out malignancy or pregnancy.
In some women, withdrawal bleeding may not occur during the pill-free interval. If the COC has been taken as described in section 4.2, it is unlikely that the pregnancy is established. However, if prior to the withdrawal bleeding the COC has not been taken correctly or if two withdrawal bleeds have not occurred, pregnancy must be ruled out before continuing to take the COC.
Chloasma may occasionally occur while taking COCs, especially in women with a history of chloasma gravidarum; patients with a tendency to chloasma should avoid exposure to the sun or ultraviolet radiation.
The onset or worsening of the conditions listed below has been reported both during pregnancy and while taking COCs; however, there is no conclusive evidence regarding the correlation between these conditions and COCs: jaundice and / or pruritus from cholestasis, formation of gallstones, porphyria, systemic lupus erythematosus, uraemic-haemolytic syndrome, Sydenham's chorea, herpes gestationis, hearing loss from otosclerosis.
In women with hereditary angioedema, exogenous estrogens can induce or aggravate the symptoms of angioedema.
Reduction or loss of efficacy
The efficacy of COCs may decrease in case of forgetting to take tablets (section 4.2), in case of vomiting and / or diarrhea (section 4.2) or in case of concomitant use of other medicinal products (section 4.5).
Preparations of hypericum perforatum should not be taken concomitantly with medicines containing oral contraceptives, digoxin, theophylline, carbamazepine, phenobarbital, phenytoin due to the risk of decreased plasma levels and decreased therapeutic efficacy of oral contraceptives, digoxin, theophylline, carbamazepine, phenobarbital, phenytoin (see section 4.5).
Reduced cycle control
Irregular blood loss (spotting or breakthrough bleeding) may occur with all oral estrogen progestins, especially in the first months of use. Thus, evaluation of any irregular blood loss becomes meaningful after an adjustment period of approximately three treatment cycles.
If irregular blood loss persists or occurs after previously normal cycles, non-hormonal causes should be considered and appropriate diagnostic measures should be taken to rule out malignancy or pregnancy. Such diagnostic measures may include a biopsy.
Some women may not experience contraceptive withdrawal bleeding during the off days. If oral estrogen has been taken as directed in section 4.2, it is unlikely that the patient is pregnant. However, if oral estrogen has not been taken as directed prior to the missed period, or if two menstruation, pregnancy must be ruled out before continuing oral estrogen progestogen use.
Information on some excipients
Ginoden contains lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp Lactase deficiency, or glucose-galactose malabsorption should not take this medicine.
Ginoden contains sucrose. Patients with rare hereditary problems of fructose intolerance and sucrase isomaltase insufficiency should not take this medicine.
04.5 Interactions with other medicinal products and other forms of interaction
Effects of other drugs on Ginoden
Interactions with other drugs that induce microsomal enzymes, resulting in increased clearance of sex hormones, can lead to breakthrough bleeding and / or contraceptive failure.
Women undergoing treatment with one of these drugs must temporarily use a barrier method or another method of contraception in addition to the combined oral contraceptive. The barrier method should be used for the entire time of concomitant intake and for 28 days following discontinuation of therapy. If concomitant drug administration continues after the end of a COC pack, the next COC pack should be started without observing the usual tablet-free interval.
The following interactions have been reported in the literature.
Substances that increase the clearance of COCs (decreased efficacy of COCs by enzyme induction) for example:
Phenytoin, primidone barbiturates, carbamazepine, rifampicin, rifabutin and there are also suspicions for oxycarbamazepine, topiramate, felbamate, griseofulvin and products containing "St. John's wort" (Hypericum perforatum).
Preparations based on Hypericum perforatum should not be administered simultaneously with oral contraceptives, as this could lead to a loss of contraceptive efficacy. Unwanted pregnancies and resumption of the menstrual cycle have been reported. This is due to the induction of enzymes responsible for the metabolism of drugs from Hypericum perforatum-based preparations. The induction effect may persist for at least 2 weeks after stopping treatment with Hypericum perforatum products.
Substances with variable effect on COC clearance, for example:
When given with COCs, some HIV / HCV protease inhibitors (e.g. ritonavir) and non-nucleoside reverse transcriptase inhibitors (e.g. nevirapine) may increase or decrease plasma concentrations of estrogens and progestogens. These changes may be clinically relevant in some cases.
• Substances that reduce the clearance of COCs (enzyme inhibitors)
Plasma concentrations of estrogen, progestogen or both may be increased by strong or moderate inhibitors of CYP3A4 such as azole antifungals (e.g. itraconazole, voriconazole, fluconazole), verapamil, macrolides (e.g. clarithromycin, erythromycin), diltiazem and grapefruit juice.
Etoricoxib doses of 60 to 120 mg / day have been shown to increase plasma concentrations of ethinylestradiol by 37% and 60% respectively when taken concomitantly with a combined hormonal contraceptive containing 0.035 mg ethinylesteradiol.
Effects of COCs on other medicinal products
Oral contraceptives can affect the metabolism of other drugs. Consequently, plasma and tissue concentrations may increase (e.g. cyclosporine) or decrease (e.g. lamotrigine).
Associations not recommended
Modafinil: risk of reduced contraceptive efficacy during treatment and for the cycle following discontinuation of treatment.
Associations to be evaluated
In case of long-term treatment with hepatic enzyme inducers, it is recommended to increase the dose of contraceptive steroids. If a high dose of oral contraceptive is not indicated or seems unsatisfactory or unreliable, for example in case of irregular periods, the use of another contraceptive method should be recommended.
Flunarizine: risk of galactorrhea due to the increased sensitivity of the breast tissue to prolactin due to the action of flunarizine.
Administration of a hormonal contraceptive containing ethinylestradiol results in a slight increase in the plasma concentration of CYP3A4 substrates (e.g. midazolam), while the plasma concentrations of CYP1A2 substrates (e.g. theophylline, melatonin and tizanidine) and CYP2C19 substrates (e.g. . omeprazole) may increase significantly.
In vitro, ethinylestradiol is a reversible inhibitor of CYP2C19, CYP1A1 and CYP1A2 as well as an irreversible inhibitor of CYP3A4 / 5, CYP2C8 and CYP2J2.
Other forms of interaction
Laboratory tests
The use of contraceptive steroids can influence the results of some laboratory tests including biochemical parameters of hepatic, thyroid, adrenal and renal function, plasma levels of transport proteins, for example of corticosteroid-binding globulin and of lipid / lipoprotein fractions , parameters of glucose metabolism, coagulation and fibrinolysis.The variations are generally within the range of normal laboratory values.
04.6 Pregnancy and lactation
Pregnancy
The product is not indicated during pregnancy.
In the event of pregnancy occurring while using Ginoden, the product must be discontinued immediately. Extensive epidemiological studies have not revealed any increased risk of birth defects in children born to women who used oral contraceptives prior to pregnancy. nor of teratogenic effects in case of accidental use of oral contraceptives during pregnancy.
The increased risk of thromboembolism in the postpartum period should be taken into account when Ginoden is restarted (see sections 4.2. And 4.4).
So far, in clinical use, and unlike diethylstilbestrol, the results of numerous epidemiological studies allow us to consider reduced the risk of malformations with estrogens administered at early pregnancy, alone or in combination.
Furthermore, the risks related to the sexual differentiation of the fetus (in particular female), which have been described with the first highly androgenomimetic progestogens, cannot be extrapolated to the more recent progestogens (such as that used in this medicinal product), which are markedly less, or not at all, androgenomimetics.
Consequently, the discovery of a pregnancy in a patient taking an "estrogen-progestogen combination" does not justify the abortion.
Feeding time
Breastfeeding can be influenced by COCs, as they can reduce the quantity and change the composition of breast milk. The use of COCs should therefore be discouraged until the end of breastfeeding. Small amounts of steroids. contraceptives and / or their metabolites may be excreted in milk but there is no evidence that this affects the health of the baby.
04.7 Effects on ability to drive and use machines
No studies on the ability to drive and use machines have been performed.
No effects on the ability to drive and use machines were observed in users of oral contraceptives.
04.8 Undesirable effects
Description of some adverse reactions
An increased risk of arterial and venous thrombotic and thromboembolic events, including myocardial infarction, stroke, transient ischemic attacks, venous thrombosis and pulmonary embolism has been observed in CHC users, and this risk is discussed in more detail in section 4.4.
Undesirable effects that have been reported in COC users.
The more appropriate MedDRA term was used to describe a specific reaction. Synonyms and related conditions are not on the list, but must be taken into consideration.
In women with hereditary angioedema, exogenous estrogens can induce or aggravate the symptoms of angioedema.
There is an increased risk of venous thromboembolism (VTE) for all women using a combined oral contraceptive. For information on the differences in risk between COCs, see section 4.4.
The following side effects have been reported in women using COCs:
- Relatively rare side effects which however require discontinuation of treatment:
- arterial thromboembolic accidents (in particular myocardial infarction, cerebrovascular accident);
- venous thromboembolic accidents (phlebitis, pulmonary embolism);
- hypertension, coronary heart disease;
- hyperlipidemia (hypertriglyceridemia and / or hypercholesterolemia);
- severe mastodynia, benign mastopathy;
- exacerbation of epilepsy;
- hepatic adenoma, cholestatic jaundice;
- chloasma.
? More common side effects that do not generally require discontinuation of treatment, but for which the use of an alternative oral contraceptive combination may be considered:
- heaviness in the legs;
- intermenstrual bleeding, oligomenorrhea, amenorrhea;
? Rarely:
- skin disorders (acne, seborrhea, hypertrichosis, rash).
? Other side effects: biliary lithiasis.
? Effects on discontinuation of treatment: post-treatment amenorrhea.
Amenorrhea with no ovulation (occurring more frequently in women with previous cycle irregularities) may be observed when treatment is discontinued. It usually resolves spontaneously. If this continues, investigations into the possibility of pituitary disorders are advisable before any further prescription.
Reporting of suspected adverse reactions
Reporting of suspected adverse reactions occurring after authorization of the medicinal product is important as it allows continuous monitoring of the benefit / risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system. "address www.agenziafarmaco.gov.it/it/responsabili.
04.9 Overdose
No serious adverse effects from overdose have been reported.
In this circumstance, symptoms such as nausea, vomiting and, in women, withdrawal bleeding may occur.
There are no antidotes and any further treatment should be symptomatic.
05.0 PHARMACOLOGICAL PROPERTIES
05.1 Pharmacodynamic properties
Pharmacotherapeutic group: progestogens and estrogens, fixed combinations.
ATC code: G03AA10.
The contraceptive effect of Ginoden is based on the interaction of several factors, the most important of which are believed to be the inhibition of ovulation and changes in the cervical mucus.
05.2 Pharmacokinetic properties
• Gestodene
Absorption
Gestodene, administered orally, is rapidly and completely absorbed. Maximum serum levels of 4 ng / ml are reached approximately 1 hour after oral administration. Bioavailability is approximately 99%.
Distribution
Gestodene is bound to serum albumin and sex hormone binding globulin (SHBG). Only 1-2% of the total concentration is present as a free steroid, about 50-70% is specifically linked to SHBG. The increase in SHBG, induced by ethinylestradiol, affects the ratio of gestodene bound to serum proteins, causing an increase in the SHBG-bound fraction and a decrease in the albumin-bound fraction. The apparent volume of distribution of gestodene is approximately 0.7 l / kg.
Metabolism
Gestodene is completely metabolised by the known metabolic pathway of steroids. Metabolic clearance from serum is approximately 0.8 ml / min / kg. When gestodene is administered with ethinylestradiol, no direct interactions were found.
Elimination
Serum gestodene levels decrease in two stages. The terminal phase is characterized by a "half-life of approximately 12-15 hours. Gestodene is not eliminated in a modified form. Its metabolites are eliminated in the faeces and urine in a ratio of approximately 6 to 4. The" half-life of " metabolite excretion is approximately 1 day.
Steady State Conditions
The pharmacokinetics of gestodene are influenced by SHBG levels, which increase approximately 3-fold when administered with ethinylestradiol. Following daily administration of the drug serum levels increase approximately four-fold reaching a steady state during the second half of the year. course of treatment.
• Ethinylestradiol
Absorption
Ethinylestradiol, administered orally, is rapidly and completely absorbed. Maximum serum levels, corresponding to 80 pg / ml, are reached within 1-2 hours after intake. During absorption and first passage in the liver, ethinylestradiol is further metabolised, resulting in an average oral bioavailability of approximately 45%, with large individual variations of approximately 20-65%.
Distribution
Ethinylestradiol is bound mainly, but not specifically, to serum albumin (approximately 98%) and induces an increase in the serum concentration of SHBG. The apparent volume of distribution has been reported to be approximately 2.8-8.6 L / kg.
Metabolism
Ethinylestradiol is subject to presystemic conjugation both in the intestinal mucosa and in the liver. Ethinylestradiol is mainly metabolised by aromatic hydroxylation, but a large variety of hydroxylated and methylated metabolites are formed, these are present as free metabolites and as conjugates with glucuronides and sulphates. The metabolic clearance of ethinylestradiol is between 2.3-7 ml / min / kg.
Elimination
Serum levels of ethinylestradiol decrease in two phases characterized by half-lives of approximately 1 hour and approximately 10-20 hours, respectively. Ethinylestradiol is not eliminated in modified form, the metabolites of ethinylestradiol are eliminated in faeces and urine in a ratio of about 4 to 6. The half-life of metabolite excretion is about 1 day.
Steady State Conditions
In accordance with the variable half-life of the terminal disposition phase from serum and daily intake, the steady state of the serum levels of ethinylestradiol are reached after about one week.
05.3 Preclinical safety data
Long-term toxicity studies with repeated doses for the evaluation of a possible oncogenic activity do not reveal tumorigenic potential in the case of therapeutic use of the preparation in humans. hormone-dependent tumors.
06.0 PHARMACEUTICAL INFORMATION
06.1 Excipients
Lactose monohydrate, corn starch, povidone 25, sodium calcium edetate, magnesium stearate, sucrose, povidone 90, macrogol 6,000, calcium carbonate, talc, ethylene glycol ester of montanic acid (E wax).
06.2 Incompatibility
Not relevant.
06.3 Period of validity
5 years.
06.4 Special precautions for storage
Do not store above 25 ° C. Store in the original package in order to protect from light.
06.5 Nature of the immediate packaging and contents of the package
Thermoformed blister, consisting of a polyvinyl chloride film and an aluminum foil sealed by heat sealing.
Calendar pack containing 21 coated tablets.
06.6 Instructions for use and handling
No special instructions for disposal.
07.0 MARKETING AUTHORIZATION HOLDER
Bayer S.p.A. - Viale Certosa, 130 - 20156 Milan (MI)
08.0 MARKETING AUTHORIZATION NUMBER
AIC n. 026435038
09.0 DATE OF FIRST AUTHORIZATION OR RENEWAL OF THE AUTHORIZATION
24.10.1987/01.06.2010
10.0 DATE OF REVISION OF THE TEXT
04/2015