Diagnosis
With an increasing degree of depth, the investigations necessary to identify thyroid tumors are objective (palpation of the neck), laboratory, instrumental and cytological. After the preliminary visit, we then proceed with a common blood test, which has the purpose of measuring the hormones produced by this gland (thyroid hormones and calcitonin), those that govern them (TSH), and the antithyroidoglobulin and antithyreoperoxidase antibodies (AbTg and AbTPO).
Through the thyroid ultrasound - thanks to the harmless ultrasounds - it is possible to study the morphology of this gland, searching for any nodules, evaluating their characteristics and collecting, if necessary, elements on their vascularization (thanks to the colordoppler technique).
The scintigraphic examination, not always necessary, exploits the small and completely harmless dose of radiation emitted by a radiopharmaceutical which - after being injected intravenously - is concentrated at the level of the thyroid allowing its functional study.
Diagnostic confirmation of thyroid cancer is obtained by a technique called fine needle aspiration, during which small samples of thyroid cells are taken to be studied in the laboratory; the sampling is performed by means of a special thin needle syringe, inserted under ultrasound guidance in the patient's neck (the examination is all in all painless, so much so that it does not normally require any type of anesthesia).
Treatment
For further information: Medicines for the treatment of Thyroid Cancer
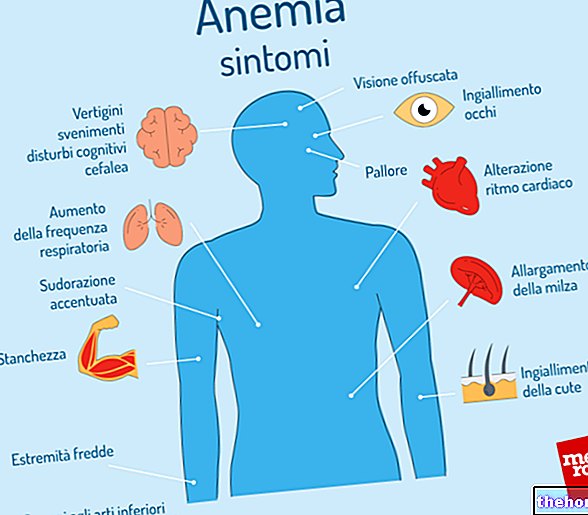
The type of treatment undertaken by the doctor, in agreement with the patient, is subject to the health conditions of the same, but also to the stage and type of disease. In the presence of malignant tumor (thyroid cancer or carcinoma), the choice generally falls on "thyroid removal surgery (thyroidectomy), which can be complete or partial (most of the gland or only one lobe can be removed - lobectomy) ) and be accompanied or not by the removal of local lymph nodes. The most evident complication of thyroidectomy is the subsequent condition of hypothyroidism (deficiency of thyroid hormones), which can be easily treated by taking a daily tablet containing these hormones (see eutirox). The therapy, however, allows the patient to lead an absolutely normal life, although especially in an initial phase it may require frequent checks (blood tests) to establish the optimal therapeutic dosage. If this is insufficient, the patient may experience symptoms such as depression, dry skin, difficulty concentrating, increased weight with water retention, constipation and a sense of cold. Conversely, when too many thyroid hormones are administered, the patient appears very thin, intolerant to heat, with moist skin, excessive emotionality, tachycardia, irritability, hand tremors and troubles of the alvus with frequent episodes of diarrhea. Replacement therapy with L-thyroxine (a synthetic analogue of the hormone produced by the thyroid) is also important to keep TSH levels below the normal range; in this way, since cancer cells express the TSH receptor, it is possible to prevent, or in any case slow down, its possible proliferation.
Additional, albeit rare, complications of thyroidectomy are hypoparathyroidism (due to damage to the parathyroid glands, with a decrease in calcemia), the consequences and complications of the wound (bleeding and infection), and possible damage to the nerves that control the vocal cords (which can cause paralysis of the same, hoarseness, decreased tone of voice or difficulty in breathing).
Patients in whom the removal of the thyroid gland (thyroidectomy) is contraindicated can be treated with radioactive iodine. This type of operation is also used to eliminate any metastases and residual thyroid tissues after surgical removal of the gland (ablation). In fact, tumor cells retain the ability to store iodine, including that present in the radiopharmaceutical. Treatment with iodine 131 is essentially based on the administration of large quantities of radioactive iodine, which are concentrated at the level of the thyroid, irreversibly damaging - and with a certain selectivity - the cells that constitute it. The risk associated with the ionizing radiation emitted by the radiopharmaceutical is reduced, but the patient is still asked to respect a series of behavioral rules at the end of the treatment (for example, avoiding close contact with pregnant women and children in the following seven days). If necessary, as happens in the forms that have already metastasized, the treatment of thyroid cancer can be combined with chemo and radiotherapy.
Other articles on "Thyroid Cancer: Diagnosis and Treatment"
- Thyroid cancer
- Thyroid Cancer - Medicines to Treat Thyroid Cancer