Generality
Proctitis is an inflammatory process affecting the rectum, typically accompanied by rectal pain, an unpleasant feeling of continual urge to defecate, small rectal bleeding, and occasionally anal discharge of mucus or pus.
Proctitis recognizes numerous possible causes of origin, such as traumatic insults, inflammatory bowel diseases and venereal or non-sexually transmitted infectious diseases.
Proctitis Symptoms
To learn more: Proctitis Symptoms

Proctitis can also be accompanied by fever, dehydration, vaginitis, vaginal discharge of bad odor, urination disorders and urethritis.
Causes and Risk Factors
There are numerous possible diseases and conditions that can trigger episodes of acute and chronic proctitis. In general, there can be distinguished causes of infectious origin (typical are food, such as salmonella, shigella and campylobacter, and sexually transmitted, such as gonorrhea, chlamydia, genital herpes, syphilis, trichomoniasis), inflammatory (such as ulcerative colitis and Crohn) and iatrogenic (radiation therapy in the treatment of pelvic tumors, abuse of laxative drugs such as bisacodyl, or antidiarrheals, and prolonged antibiotic therapies, especially with lincomycin and clindamycin).
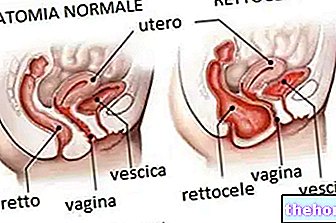
For what has been said, among the most important risk factors we remember unprotected sexual intercourse (failure to use barrier methods such as condoms), especially if of an anal nature but not only (in females, proctitis may be due to infected vaginal discharge that come into contact with the anal region), sexual promiscuity and the presence of inflammatory bowel diseases.
Complications
Possible complications of neglected or unresponsive proctitis to medical treatments include anemia (related to bleeding episodes), rectal ulcers (erosions of the intestinal mucosa) and fistulas (actual perforations of the enteric mucosa, which depending on the level at which they occur they connect normally separate structures, such as different tracts of intestine, skin and intestine, bladder and intestine or vagina and intestine).
Proctitis Diagnosis
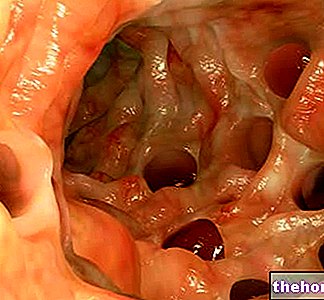
The diagnosis of proctitis can be made through tests such as rectal swab and coproculture associated with an antibiogram (allow to discover the infectious agent and its susceptibility to antibiotics), flexible sigmoidoscopy (which allows to visualize the internal walls of the rectum and sigma, possibly taking biopric fragments) and colonoscopy.
Treatment and prevention
To be effective, the treatment of proctitis cannot be separated from the correct identification of the causes of origin. If, for example, antibiotics are particularly useful in case of infectious bacterial proctitis (chlamydia, gonorrhea), they are completely useless and even dangerous in case of viral infections (genital herpes), for which antiviral drugs are possibly indicated. In case of proctitis of inflammatory origin, anti-inflammatory drugs, such as mesalamine (or 5-aminosalicylic acid), salazopyrine or corticosteroids, to be taken orally (tablets) or rectally (suppositories or enema) may be prescribed. These same drugs, together with amifostine, may also prove useful in radiation therapy proctitis.
Other articles on "Proctite"
- Proctitis Cure Medicines
- Proctite diet