Generality
We speak of placenta previa when the placenta grows at the bottom of the uterus, in correspondence with the cervix. Not all placentas previa present themselves in the same way: in some cases, the opening between the uterus and vagina is covered (more serious eventuality); in other cases, the placenta is only placed next to the opening.

Figure: comparison between a normal placenta and a placenta previa. From the site: riversideonline.com
More than a precise cause, risk factors have been recognized. The main symptom, also fundamental for the diagnosis, is the loss of blood from the vagina.
The therapy consists in adopting the most suitable measures to save the life of the mother and the fetus.
In this sense, early diagnosis and timely intervention are essential for a positive prognosis.
Brief anatomical recall: placenta and uterus
To better understand what happens in placenta previa, it is necessary to make a brief anatomical review of the placenta and the uterus.
THE PLACENTA
The placenta forms inside the uterus during pregnancy to nourish, protect and support the growth of the fetus. It is therefore a temporary or deciduous organ.
The placenta has a dual origin: maternal and fetal. The maternal component derives from the endometrium of the uterus; the fetal component corresponds to the chorionic villi.
The chorionic villi are branched extensions of the placenta, which sink into the uterus (inside the "lacunae"), to withdraw nutrients and oxygen from the mother's blood vessels. At this point, nourishment and oxygen convey towards the umbilical cord and, from there, reach the fetus.
POSITION AND DIMENSIONS OF THE PLACENTA
The placenta can grow in any position within the uterus.
At the end of pregnancy, the placenta takes on the following characteristics:
- It is blue-red in color and discoid in shape
- The diameter measures between 15 and 22 centimeters
- The thickness varies between 2 and 4 centimeters
- Weighs 500-600 grams (15% of the baby's weight)
MAIN FUNCTIONS OF THE PLACENTA
The placenta is essential for the survival and growth of the fetus. In fact, it is a multifunctional organ: it acts as a lung, kidney, digestive system, immune system and protective barrier.

THE UTERUS
The uterus is the female genital organ, which receives the fetus, during a pregnancy. It is located in the small pelvis, precisely between the bladder (anteriorly), the rectum (posteriorly), the intestinal loops (above) and the vagina (below).
Two areas can be recognized in the uterus: the body of the uterus and the cervix (or neck of the uterus).
The body is the upper portion of the uterus.
The cervix, on the other hand, is the lower portion, which connects to the vagina. It is cylindrical in shape and is provided with an opening (or orifice), between the uterus and the vagina, which allows the passage of spermatozoa, menstrual flow and the fetus (during childbirth).
What is placenta previa
By placenta previa s "means the circumstance in which the placenta grows in the lower part of the uterus, in correspondence with the cervix.

Placenta previa, together with placental abruption, is a major cause of bleeding antepartum, which, in turn, is a major reason for maternal and fetal death.
N.B: it is considered hemorrhage antepartum any vaginal blood loss occurring from the 24th week of gestation.
DEGREE OF PLACENTA PREVIA
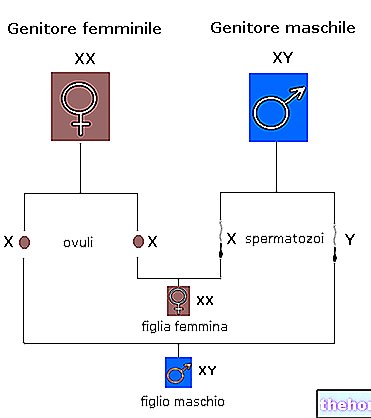
According to the position assumed by the placenta in the uterine cervix, there are four possible types of placenta previa:
Grade I
Features: the placenta does grow in the lower portion of the uterus, but is distant from the opening of the cervix, which connects the uterus and vagina.
Grade II
Features: the placenta is positioned at the edge of the utero-vaginal opening of the cervix.
Grade III
Features: the placenta covers a part of the utero-vaginal opening of the cervix.
Grade IV
Features: the placenta covers the entire utero-vaginal opening of the cervix.

Figure: the different degrees of placenta previa. It can be appreciated how grade IV completely covers the opening between the uterus and vagina.. Image from the site mala-sanita.net
The severity of placenta previa increases with increasing grade. Grade I episodes are therefore less dangerous for the survival of the mother and fetus than grade II episodes, which in turn are less dangerous than grade III or IV.
EPIDEMIOLOGY
Placenta previa, in all its manifestations, occurs with an "incidence equal to one case in every 200 pregnancies. The grade IV form, the most dangerous, is much rarer and affects one pregnant woman in every 1000.
About 1/3 of the bleeding antepartum it is caused by placenta previa, which also causes about 2-3% of perinatal deaths.
N.B: the perinatal period is the one that goes from the 27th week of gestation to the first 28 days of life of the newborn.
Causes of placenta previa
The precise cause of placenta previa is not known. However, it has been found that certain circumstances concerning the mother favor its onset. But what are these favorable situations?
RISK FACTORS
The risk factors are different and, often, to be decisive, they must be concurrent with each other. In other words, a single event may not be enough, but an "overlap of several favorable conditions" may be needed.
In the "list of risk factors, appear:
- Previous episodes of placenta previa.
- Advanced age of the mother.
Over 35-40 years old - Previous surgery on the uterus.
They are the caesarean section and the uterine fibroid surgery. - Abnormal shape of the uterus.
An "unusual anatomy of the uterus" could favor the incorrect position of the placenta - Smoking and drug abuse.
Smoking during pregnancy or using drugs, such as cocaine, predisposes women to abnormal placenta formation. - Multiple pregnancy.
In these cases, the placenta can be large and invade the cervix as a result. - Previous spontaneous or induced abortions.
MORE: Placenta Previa - Symptoms, Diagnosis and Therapy "

-cos-come-si-calcola-a-cosa-serve.jpg)




.jpg)


















