Generality
Keratoconus is a disease that causes deformation of the cornea (transparent ocular surface placed in front of the iris, which functions as a converging lens allowing the correct passage of light towards the internal structures of the eye).

Keratoconus does not allow the correct passage of light towards the internal ocular structures and modifies the refractive power of the cornea, causing a distortion in vision.
Symptoms
For further information: Keratoconus Symptoms
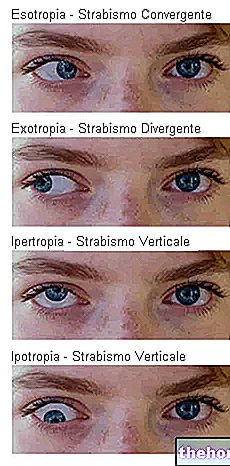
Keratoconus is a slowly progressive disease. The deformation of the cornea can affect one or both eyes, even if the symptoms on one side can be markedly worse than on the other (the disease can present itself in bilateral asymmetrical form).

Symptoms of keratoconus can include:
- Distorted vision;
- Increased sensitivity to light (photophobia);
- Mild eye irritation;
- Blurred vision
- Double vision with one eye closed (monocular polyopia).
Keratoconus often progresses slowly over the course of 10-20 years before stabilizing.
During the evolution of the condition, the most common manifestations are:
- Visual acuity impaired at all distances;
- Reduced night vision;
- Increased myopia or kerotocone astigmatism;
- Frequent changes in eyeglass prescription
- Inability to wear traditional contact lenses.
Occasionally, keratoconus can advance more rapidly, causing corneal edema and scarring. The presence of scar tissue on the surface of the cornea determines the loss of its homogeneity and transparency; as a result, opacity can occur, which significantly reduces vision.
Corneal abnormalities or lesions associated with keratoconus can significantly affect the ability to perform simple tasks, such as driving, watching television, or reading a book.
Causes
The exact cause of keratoconus is not yet known. Some researchers believe that genetics play an important role, as it is estimated that around 10-15% of affected people have at least one family member with the same condition (evidence of transmission genetics).
Additionally, keratoconus is often associated with:
- corneal injury or damage: vigorous eye rubbing, chronic irritation, wearing contact lenses for prolonged periods, etc.
- Other eye conditions, including: retinitis pigmentosa, retinopathy of the premature baby, and vernal keratoconjunctivitis.
- Systemic diseases: Leber congenital amaurosis, Ehlers-Danlos syndrome, Down syndrome and osteogenesis imperfecta.
Some researchers believe that an imbalance in enzymatic activity within the cornea may make it more vulnerable to oxidative damage from free radicals and other oxidizing species. Particular proteases show signs of increased activity and work by breaking part of the cross-links between the collagen fibers in the stroma (the deepest part of the cornea). This pathological mechanism would produce a weakening of the corneal tissue, with a consequent reduction in thickness and biomechanical resistance.
Diagnosis
Early diagnosis can prevent further damage and vision loss. During a routine eye exam, doctors ask the patient questions about visual symptoms and any family predisposition, then check for irregular astigmatism and other problems by measuring the refraction of the eye. The ophthalmologist may ask you to look through a device to determine which combination of optical lenses allows for the sharpest vision. A keratometer is used to measure the curvature of the outer surface of the cornea and the extent of refractive defects. In severe cases, this tool may not be sufficient to make a correct diagnosis.
Further diagnostic tests may be needed to determine the shape of the cornea. These include:
- Retinoscopy: evaluates the projection and reflection of a light beam on the patient's retina, examining how it is focused on the back of the eye, even with the forward and backward tilt of the light source. Keratoconus is among the ocular conditions that show a scissor reflex (two bands approach and distance themselves like the blades of a pair of scissors).
- Slit-lamp examination: If a suspicion of keratoconus emerges from retinoscopy, this examination can be performed. The doctor directs a beam of light into the eye and uses a low-power microscope to view eye structures and look for potential defects in the cornea or other parts of the eye. The slit lamp exam evaluates the shape of the corneal surface and looks for other specific features of keratoconus, such as the Kayser-Fleischer ring. This consists of a yellow-brown-greenish pigmentation at the periphery of the cornea, caused by the deposition of hemosiderin within the corneal epithelium and evident on examination with a cobalt-blue filter. The Kayser-Fleischer ring is present in 50% of keratoconus cases. The test can be repeated after administration of mydriatic eye drops to dilate the pupils and visualize the back of the cornea.
- Keratometry: This non-invasive technique projects a series of concentric rings of light onto the cornea. The ophthalmologist measures the reflection of the light beams to determine the curvature of the surface.
- Corneal topography (corneal mapping): This diagnostic investigation allows you to generate the topographic map of the anterior surface of the eye. A computerized optical instrument is used to project light patterns onto the cornea and measure its thickness. When the keratoconus is in its early stages, corneal topography shows any distortions or scars on the cornea Alternatively, optical coherence tomography (OCT) can be used.
Treatment
Treatment of keratoconus often depends on the severity of the symptoms and how fast the condition is progressing.During the initial phase, the visual defect can be corrected with prescription glasses and soft or semi-rigid contact lenses. However, over time the disease inevitably thins the cornea, giving it an increasingly irregular shape that could make these devices no longer sufficient. Advanced keratoconus may require a cornea transplant.