The cardiovascular system consists of three elements:
blood - a fluid that circulates through the body and that carries substances to the cells and removes others;
blood vessels - conduits through which blood circulates;
the heart - a muscular pump that distributes blood flow in the vessels.
The cardiovascular system can distribute substances throughout the body faster than diffusion can, as molecules in the blood move around the circulating liquid like water particles in a river. In the bloodstream, the molecules move faster because they do not proceed randomly, back and forth or zigzag as in diffusion, but in a precise and orderly manner.
The circulation of blood is so crucial to our existence that if the blood flow stops at a certain moment, we will lose consciousness within a few seconds and expire after a few minutes. Obviously the heart must perform its function continuously and correctly, every minute and every day of our life.
Heart
The heart is contained in the center of the rib cage, located anteriorly and slightly displaced to the left. Its shape roughly resembles that of a cone, the base of which faces upward (right), while the tip points downward, to the left.
The myocardium, that is the heart muscle, allows the heart to contract, sucking blood from the periphery and pumping it back into the circulation.
Internally, the heart is lined with a serous membrane called the endocardium. Externally, however, the heart is contained in a membranous sac called the pericardium, which constitutes the space within which the heart is free to contract, without necessarily giving rise to friction with the surrounding structures. The cells of the pericardium secrete a liquid which has the task of lubricating the surfaces to avoid such friction.
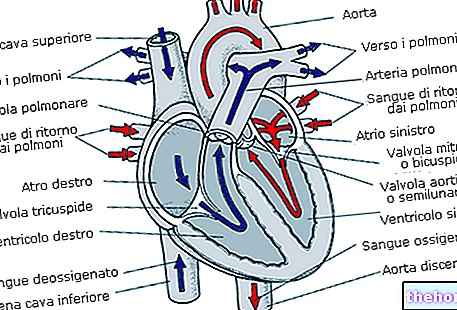
The heart cavity is divided into four areas: two atrial areas (right atrium and left atrium) and two ventricular areas (right ventricle and left ventricle).
The two right cavities (atrium and ventricle) are communicating with each other thanks to the right atrio-ventricular orifice, which is cyclically closed by the tricuspid valve. The two left cavities are in communication through the left atrio-ventricular orifice, closed cyclically from the bicuspid or mitral valve.

The right cavities are completely separated from the left cavities; this separation occurs by two septa: the interatrial one (which separates the two atria) and the interventricular one (which separates the two ventricles).
The functioning of the tricuspid valve (formed by three connective flaps) and that of the mitral valve (formed by two connective flaps) allow the blood to flow in only one direction, starting from the atria, up to the ventricles, and not vice versa.
The right ventricle originates from the pulmonary artery, and is separated from this by the pulmonary valve (consisting of three connective flaps). The left ventricle is separated from the aorta by the aortic valve, which has a completely overlapping morphology to the pulmonary valve.
These two valves allow blood to flow from the ventricle to the blood vessel (pulmonary artery and aorta), without this changing direction.
The right atrium receives blood from the periphery through two veins: the superior vena cava and the inferior vena cava. This blood, called vena, is poor in oxygen and reaches the heart muscle precisely to re-oxygenate. On the contrary, the left atrium receives blood arterial (oxygen-rich) from the four pulmonary veins, so that the same blood can be poured into the circulation and perform its functions: re-oxygenate and nourish the various tissues.
The heart, like the skeletal muscles, contracts in response to an electrical stimulus: for the skeletal muscles this stimulus arrives from the brain through the various nerves; for the heart, on the other hand, the impulse is formed autonomously, in a structure called the sino-atrial node, from where the electrical impulse reaches the atrio-ventricular node.
From the atrio-ventricular node originates the bundle of His, which conducts the impulse downwards; the bundle of His divides into two branches, the right and the left, which descend respectively on the right and left side of the interventricular septum. These bundles progressively branch out, reaching, with their ramifications, the whole ventricular myocardium, where the electrical impulse produces the contraction of the heart muscle.
The small circulation
The small circulation begins where the large one ends: the venous blood from the right atrium descends into the right ventricle, and here, through the pulmonary artery, carries the blood to each of the two lungs. Inside the lung, the two branches of the pulmonary artery divide into smaller and smaller arterioles, which become, at the end of their path, pulmonary capillaries. The pulmonary capillaries flow through the pulmonary alveoli, where the blood, poor in O2 and rich in CO2, is re-oxygenated.
It is interesting to note how in the pulmonary circulation the veins carry arterial blood and the arteries venous blood, contrary to what happens in the systemic circulation.
The great circle starts from the aorta and ends at the capillaries
The aorta, through successive branches, gives rise to all the minor arteries that reach the various organs and tissues. These branches become progressively smaller and smaller, until they become capillaries responsible for the exchange of substances between blood and tissues. supplied to the cells with nutrients and oxygen.
ELEMENTS OF CARDIOVASCULAR PHYSIOLOGY
The heart has four basic properties:
1) the ability to contract;
2) the ability to self-stimulate at certain heart rates;
3) the ability of myocardial fibers to transmit the electrical stimulus received to neighboring ones, also making use of preferential conduction pathways;
4) excitability, that is the ability of the heart to respond to the electrical stimulus that has been administered.
The cardiac cycle is the time between the end of one cardiac contraction and the beginning of the next. In the cardiac cycle we can distinguish two periods: diastole (the period of relaxation of the myocardial muscles and filling of the heart) and systole (period contraction, ie the expulsion of blood into the systemic circulation through the aorta).
From the sino-atrial node the electrical impulse reaches the atrio-ventricular node, where it undergoes a slight slowdown and where it spreads, following the two branches of the bundle of His (and their terminal branches), to the entire ventricular myocardium, causing it to contract .
Most (about 70%) of the blood that reaches the heart during diastole passes directly from the atria to the ventricles, while the remainder is pumped from the atria to the ventricles by contracting the atria at the end of diastole. This last amount of blood is not of particular importance in conditions of rest; it becomes indispensable during exertion when the increase in heart rate shortens the diastole (ie the period of filling of the heart) making the time available for the filling of the ventricles. During atrial fibrillation (i.e. that condition in which the heart beats in a completely irregular way) there is a functional limitation of cardiac performance, which manifests itself particularly during exertion.
The time that elapses between the closing of the atrioventricular valves and the opening of the semilunar ones is called the isometric contraction time, because, even if the ventricles enter into tension, the muscle fibers do not shorten.
At the end of the systole, the ventricular muscles relax: the endoventricular pressure falls to much lower levels than those present in the aorta and pulmonary artery, causing the closing of the semilunar valves and, subsequently, the opening of the atrioventricular ones (because the intra-ventricular pressure became lower than intra-atrial pressure).
The period between the closing of the semilunar valves and the opening of the atrioventricular valves is called the isovolumetric relaxation period, as the muscle tension collapses, but the volume of the ventricular cavities remains unchanged. When the atrioventricular valves open, the blood flows again. from the atria to the ventricles and the described cycle begins again.
The movement of the heart valves is passive: they open and close passively as a consequence of the pressure regimes existing in the chambers separated from the valves themselves. The function of these valves is therefore to allow the flow of blood in a "single direction, the antegrade one, preventing the blood from turning back.
Other articles on "The Cardiovascular System"
- athlete's heart
- cardiological examinations
- cardiovascular pathologies
- Congenital aortic stenosis; aortic coarctation; stenosis and mitral insufficiency
- cardiovascular pathologies 3
- cardiovascular pathologies 4
- electrocardiographic abnormalities
- electrocardiographic abnormalities 2
- electrocardiographic abnormalities 3
- ischemic heart disease
- screening of the elderly
- competitive fitness
- cardiovascular sports commitment
- cardiovascular commitment sport 2 and BIBLIOGRAPHY











.jpg)











