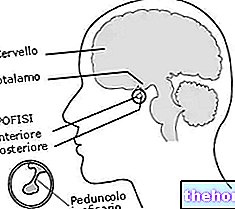
So is the pituitary
The pituitary or pituitary gland is a very small anatomical structure with enormous biological importance.
Despite dimensions similar to a bean and a practically negligible weight (just over half a gram), the pituitary gland controls the functionality of numerous organs, including thyroid, cortical portion of the adrenal glands and gonads (ovaries and testicles).

How does it work
Pituitary hormones
In all, the pituitary gland produces nine hormones, of which seven in its anterior portion and two in the posterior one. The pituitary gland in fact consists of two parts:
- an anterior part, called the adenohypophysis,
- a posterior part, called neurohypophysis (between which there is an intermediate portion).
This distinction is not only anatomical or didactic, since the functions and embryonic origins are also different.
Hypothalamic Control of the Pituitary
The pituitary is located inside the skull, more precisely at the base of the diencephalon, behind the optic chiasm. Protected by a depression of the sphenoid bone, the sella turcica, it anchors to the lower region of the hypothalamus by means of the infundibulum, otherwise known as the pituitary peduncle; the activity of the pituitary gland, in fact, is controlled by the hypothalamus itself, which through neurons specialized produces and releases peptides capable of promoting (RH Releasing Hormone) or inhibit (IH Inhibiting Hormone) the release of related pituitary hormones. Each hypothalamic factor is specific for a pituitary hormone; for example, GHRH (growth hormone release factor) stimulates the pituitary gland to produce GH, while the hypothalamic hormone TRH increases the pituitary release of TSH, which in turn stimulates the thyroid to produce thyroid hormones.

Thanks to hypothalamic factors, therefore, the nervous system directly controls the endocrine system; this regulation is allowed by the so-called pituitary portal system, a vascular structure that transfers the hypothalamic factors of release and inhibition to the adenohypophysis.
Each portal system consists of two capillary beds joined by a vessel; specifically, the hypothalamus-pituitary system arises from the two superior pituitary arteries (belonging to the circle of Willis) which send branches into the pituitary peduncle, where they capillarize.
The axons of the parvicellular neurons terminate on this first capillary bed, freeing their RH and IH there. The venules that arise from these capillaries flow into the junction veins (pituitary veins) which go to the adenohypophysis crossing the peduncle; here, branching off, they form a second capillary bed in the anterior portion of the gland. Coming into contact with the adenohypophyseal cells, these capillaries yield on the one hand the Releasing and Inhibiting Hormons and on the other collect the corresponding adenohypophyseal hormones. The products of the anterior pituitary gland are then introduced into the secondary capillary plexus and from there, through drainage veins that enter the cavernous sinuses of the dura mater, reach the general circulation until they meet the target organ.
Anterior pituitary or adenohypophysis
The anterior pituitary or adenohypophysis constitutes 80% by weight of the pituitary gland; secretes, under direct command of the hypothalamus, a series of hormones called pituitary tropins:
- thyroid-stimulating hormone or TSH: produced by thyrotropic cells, its target organ is the thyroid, in which it stimulates the production of thyroid hormones (T3 and T4, better known as triiodothyronine and thyroxine).
- Adrenocorticotropic hormone or ACTH: produced by corticotropic cells, it stimulates the release of hormones that act in the cortical portion of the adrenal gland, stimulating the secretion of glucocorticoids, such as cortisol, which participate in the regulation of glucose metabolism.
- Follicle stimulating hormone or FSH: produced by gonadotropic cells, it stimulates the ovarian follicular cells to produce estrogen (estradiol), while in the male it controls spermatogenesis at the testicular level.
- Stimulating luteum hormone (luteotropic) or LH: produced by gonadotropic cells, it induces ovulation and the transformation of the follicle that expelled the egg into the corpus luteum; the cells of the latter produce progesterone in view of the possible pregnancy. In humans, luteotropic hormone stimulates interstitial (Leydig) cells to produce androgens (testosterone).
- Prolactin or PRL: produced by lactotropic cells, it participates - in synergy with other hormones (estrogen, progesterone, glucocorticoids and placental hormones - in the development of the mammary gland and in the production of milk. In the male it stimulates the activity of the prostate.
- Somatotropic hormone or GH: produced by the somatotropic cells of the anterior pituitary, it is also known as growth hormone or somatotropin (STH); it has an anabolic effect by influencing protein metabolism and stimulating body growth (especially at the muscular and skeletal level). It also increases lipid catabolism and saves glucose.
The anterior pituitary or adenohypophysis is made up of three parts (pars or lobes): pars tuberalis (constitutes the peduncle of the pituitary), pars intermedia (pituitary intermedia) and pars distalis (the largest). In the "context of this last portion" - also known as the anterior lobe since it represents the qualitatively most important part of the gland - there are cells with different dyeing affinities for dyes, as such distinct in chromophobic cells (undifferentiated elements or without secretory activity ) and chromophilic cells; the latter are classified into acidophilic cells, which secrete protein hormones (GH, PRL) and appear more pink, and basophilic cells, which secrete glycoprotein hormones (ACTH, TSH, FSH, LH) and appear paler.
posterior pituitary "













.jpg)











