It has been known for a century now that lymphocytes are activated in the blood before and during exercise; however, the concentration of lymphocytes is considerably reduced after the exercise itself.
There is therefore a general decline in the activity of the immune system in the post-exercise phase; this phenomenon, defined as "open window", is detectable in various conditions of physical stress, such as exercise, surgery, burns, trauma , acute myocardial infarction and severe infections.
During the "open window" phase, the subject finds himself in a situation of particular risk of infections.
water of the showers, the conditioned air of the environments or of the means of transport, represent an optimal vehicle through which potentially infectious agents can be contracted.
The "open window" phase has an extremely variable duration both in the subject and in the population; it stands at times ranging between 3 and 72 hours, depending on the basal immune level of the subject and materializes in a high risk of infections during intensive training or during the two weeks following sporting events of particular athletic commitment.
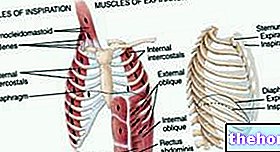
There are also several contributing causes that contribute to raising the athlete's susceptibility to infections: high respiratory rates, the consequent dryness of the oral mucous membranes and the increase in mucus viscosity, lead to a reduced clearance at the nasal and tracheal level; dietary factors and insufficient intake of essential nutritional components (glutamine, arginine, L-carnitine, essential fatty acids, vitamin B6, folic acid, vitamin E) can reduce lymphocyte mobilization.
Muscle microtraumas, even if at an early stage lead to the expression of the C reactive protein and other factors that stimulate immune functions, then lead to a leukocyte sequestration at the site of the trauma itself and the release of free radicals.
Trauma-related issues should not be underestimated, as their impact on the immune system can be significant; moreover, the desire to resume physical activity as soon as possible or, in the case of the professional athlete, the need to honor pressing competitive commitments and contracts stipulated by demanding sponsors, induces to try the path of rapid rehabilitation and a return to uncompleted healing activity.
they are diverted towards the site of the lesion, therefore unavailable for a complete immune function.
It has also been observed how a high blood concentration of catecholamines, adrenaline and noradrenaline, corresponds to the phases of greater lymphocyte activation, while the phase following exercise, frankly cortisolic, corresponds to the reduction of lymphocyte concentration.
Since the secretion of endogenous cortisol is influenced by circadian rhythms, in the same subject, the impact of the post-physical stress cortisol phase on "open window" it can be variable according to the different hours of the day.
This shows that there is a link between psychological stress, the endocrine system, the nervous system and the immune system.
It is interesting to note that both light intensity or duration physical exercise and more intense and prolonged exercises are able to activate lymphocytes in the blood, but only prolonged (> 1 hour) and / or high intensity (> 70) efforts. % VO2 max) produce immunosuppression in the post-exercise phase.
For this reason the risk of infections, especially of the upper airways, varies greatly according to physical activity, being minimal in conjunction with moderate physical activity and higher in sedentary subjects or subjected to intense activity.
Keep reading...
Edited by Doctor Alessio Capobianco
Second part: Competitive activity, stress and vaccinations