Active ingredients: Olmesartan, Amlodipine
BIVIS 20 mg / 5 mg film-coated tablets
BIVIS 40 mg / 5 mg film-coated tablets
BIVIS 40 mg / 10 mg film-coated tablets
Why is Bivis used? What is it for?
Bivis contains two substances called olmesartan medoxomil and amlodipine (as amlodipine besylate). Both are used to control hypertension.
- Olmesartan medoxomil belongs to a group of medicines called 'angiotensin II receptor antagonists'. They lower blood pressure by releasing blood vessels.
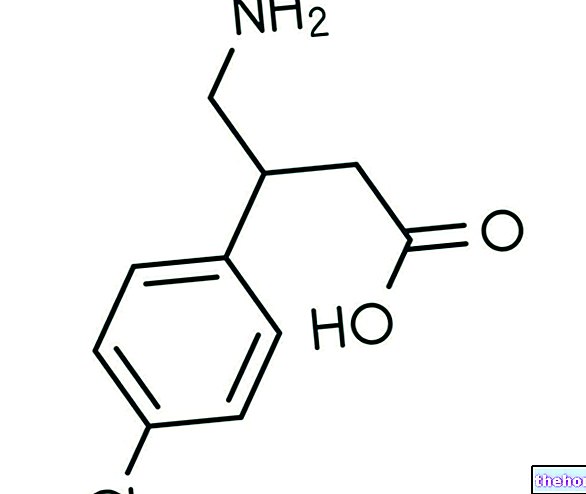
- Amlodipine belongs to a group of substances called "calcium channel blockers". Amlodipine prevents calcium from entering the vessel wall by counteracting blood pressure and reducing blood pressure.
The action of both substances helps to counteract vascular tension, so that the vessels are released and blood pressure is reduced.
Bivis is used to treat high blood pressure (also called "arterial hypertension") in patients whose blood pressure is not sufficiently controlled by olmesartan medoxomil or amlodipine alone.
Contraindications When Bivis should not be used
Do not take Bivis
- if you are allergic to olmesartan medoxomil or amlodipine or to a particular group of calcium channel blockers, the dihydropyridines, or to any of the other ingredients of this medicine (listed in section 6). If you think you are allergic, talk to your doctor before taking Bivis.
- if you are more than three months pregnant (it is better to avoid taking Bivis even in early pregnancy - see "pregnancy and breastfeeding" section).
- if you have diabetes or impaired kidney function and you are being treated with a blood pressure lowering medicine containing aliskiren.
- if you have severe liver problems, if bile secretion is impaired or its flow from the gallbladder is blocked (for example by gallstones) or if you experience jaundice (yellowing of the skin and eyes)
- if your blood pressure is very low.
- if you have insufficient blood supply to tissues with symptoms such as low blood pressure, weak pulse, fast heart beat (shock, including cardiogenic shock). Cardiogenic shock means shock due to severe heart problems.
- if the blood flow from your heart is blocked (for example due to a narrowing of the aorta (aortic stenosis)).
- if you suffer from reduced cardiac output (causing shortness of breath or peripheral swelling) after a heart attack (acute myocardial infarction)
Precautions for use What you need to know before taking Bivis
Talk to your doctor or pharmacist before taking Bivis.
Consult your doctor if you are taking any of the following medicines used to treat high blood pressure:
- an "ACE inhibitor" (eg enalapril, lisinopril, ramipril), particularly if you have diabetes-related kidney problems.
- aliskiren
Your doctor may check your kidney function, blood pressure, and the amount of electrolytes (such as potassium) in your blood at regular intervals.
See also information under the heading "Do not take Bivis"
Consult your doctor if you also have any of the following health problems:
- Kidney problems or kidney transplant.
- Liver disease.
- Heart failure or problems with your heart valves or heart muscle.
- Severe vomiting, diarrhea, treatment with high doses of diuretics or if you are on a low-salt diet.
- Increased levels of potassium in the blood.
- Problems with the adrenal glands (hormone-producing glands, located above the kidneys)
Tell your doctor if you experience severe and prolonged diarrhea with significant weight loss. Your doctor will evaluate your symptoms and decide whether to continue this antihypertensive treatment.
As with any medicine that lowers blood pressure, too much blood pressure reduction in patients with circulatory disorders of the heart or brain could lead to a heart attack or stroke. Your doctor will then check your blood pressure carefully.
You should tell your doctor if you think you are pregnant (or if there is a possibility of becoming pregnant). Bivis is not recommended in early pregnancy and must not be taken if you are more than three months pregnant as it may cause serious harm to your baby if used at that stage (see "pregnancy and breastfeeding" section).
Children and adolescents (up to 18 years)
Bivis is not recommended for children and adolescents under 18 years of age.
Interactions Which drugs or foods can change the effect of Bivis
Tell your doctor or pharmacist if you are also taking or have recently taken any of the following medicines:
- Other medicines that lower blood pressure may increase the effect of Bivis Your doctor may need to adjust your dose and / or take other precautions If you are taking an ACE inhibitor or aliskiren (see also information under the heading: "Do not take Bivis" and "Warnings and precautions")
- Potassium supplements, salt substitutes that contain potassium, diuretics or heparin (to thin the blood and prevent thrombosis). The use of these medicines taken together with Bivis can increase the levels of potassium in the blood.
- Lithium (a medicine used to treat mood swings and some types of depression) used together with Bivis can increase the toxicity of lithium. If you have to take lithium, your doctor will measure your lithium blood levels.
- Non-steroidal anti-inflammatory drugs (NSAIDs, medicines used to decrease pain, swelling and other symptoms of inflammation, including "arthritis) used together with Bivis may increase the risk of kidney failure. The effect of Bivis may be reduced by NSAIDs. .
- Colesevelam hydrochloride, a medicine that reduces cholesterol levels in the blood, which may decrease the effect of Bivis. Your doctor may advise you to take Bivis at least 4 hours before colesevelam hydrochloride.
- Some antacids (used for indigestion or stomach acid) may slightly reduce the effect of Bivis.
- Medicines for HIV / AIDS (e.g. ritonavir, indinavir, nelfinavir) or for the treatment of fungal infections (e.g. ketoconazole, itraconazole).
- Diltiazem, varapamil, drugs used for heart rhythm problems and high blood pressure.
- Rifampicin, erythromycin, clarithromycin, drugs used for tuberculosis or other infections.
- St. John's wort (Hypericum perforatum), a herbal remedy
- Dantrolene (infusion for severe body temperature changes).
- Simvastatin, a substance used to reduce cholesterol and fat (triglyceride) levels in the blood. Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
Bivis with food and drink
Bivis can be taken on a full or empty stomach. The tablet should be swallowed with some liquid (such as a glass of water). If possible, take your daily dose at the same time each day, for example with breakfast.
People taking Bivis should not consume grapefruit and grapefruit juice as grapefruit and grapefruit juice can cause the levels of the active substance amlodipine to rise in the blood, which can lead to an unpredictable increase in the hypotensive effect of Bivis.
Warnings It is important to know that:
Older people
If you are over 65 years of age, your doctor will check your blood pressure regularly with each dose increase to prevent it from falling too low.
Black patients
As with other similar medicines, the blood pressure lowering effect of Bivis may be somewhat reduced in black patients.
Pregnancy and breastfeeding
Pregnancy
You should tell your doctor if you think you are pregnant (or if there is a possibility of becoming pregnant). As a rule, your doctor will advise you to stop taking Bivis before becoming pregnant or as soon as you know you are pregnant and will advise you to take another medicine instead of Bivis. Bivis is not recommended for women. "early pregnancy and must not be taken if you are more than three months pregnant, as it may cause serious harm to your baby if taken after the third month of pregnancy.
If you become pregnant while taking Bivis, please inform and see your doctor immediately.
Feeding time
Tell your doctor if you are breastfeeding or about to start breastfeeding. Bivis is not recommended for women who are breastfeeding and your doctor may choose another treatment for you if you wish to breastfeed, especially if the baby is a newborn or is born premature.
Ask your doctor or pharmacist for advice before taking any medicine if you are pregnant or breastfeeding or think you are pregnant or planning to become pregnant
Driving and using machines
You may feel sleepy, sick or dizzy or have a headache while being treated for high blood pressure. If this happens, do not drive or use machines until the symptoms have disappeared. Ask your doctor for advice.
Dose, Method and Time of Administration How to use Bivis: Posology
Always take this medicine exactly as your doctor or pharmacist has told you. If you are unsure, consult your doctor or pharmacist.
- The recommended dose of Bivis is one tablet per day.
- The tablets can be taken on a full or empty stomach. Swallow the tablets with some liquid (such as a glass of water). The tablets should not be chewed. Do not take them with grapefruit juice.
- If possible, take your daily dose at the same time each day, for example with breakfast
Overdose What to do if you have taken too much Bivis
If you take more Bivis than you should
If you take more tablets than you should, you may have low blood pressure with symptoms such as dizziness, fast or slow heart beat.
If you take more tablets than you should or if a child accidentally swallows some, go to your doctor or nearest emergency department immediately and take the medicine pack or this leaflet with you.
If you forget to take Bivis
If you forget to take a dose, just take your normal dose the next day. Do not take a double dose to make up for a forgotten dose.
If you stop taking Bivis
It is important to continue taking Bivis unless your doctor tells you to stop.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Side Effects What are the side effects of Bivis
Like all medicines, this medicine can cause side effects, although not everybody gets them. If they do occur, they are mostly mild and do not require discontinuation of treatment.
Although they do not occur in all people, the following two side effects can be serious:
During treatment with Bivis, allergic reactions may occur, which may affect the whole body, with swelling of the face, mouth and / or larynx (seat of the vocal cords), associated with itching and rash. If this happens, stop. taking Bivis and contact your doctor immediately.
Bivis can cause excessive reductions in blood pressure in sensitive individuals or as a result of an allergic reaction. This could cause severe lightheadedness or fainting. If this happens, stop taking Bivis, contact your doctor immediately and stay in a lying position.
Other possible side effects of Bivis:
Common (affects less than 1 in 10 patients):
Dizziness; headache; swelling of ankles, feet, legs, hands or arms; tiredness.
Uncommon (affects less than 1 in 100 patients):
Dizziness on standing up; lack of energy; tingling or numbness in the hands or feet; dizziness; heartbeat more marked or faster; low blood pressure with symptoms such as dizziness, light-headedness, shortness of breath; cough; nausea; vomiting; indigestion; diarrhea; constipation; dry mouth; pain in the upper abdomen; rash; muscle spasms; pain in arms and legs; back pain; feeling of urgency to urinate; sexual inactivity; inability to get or maintain an erection; weakness. Some changes in blood tests have also been observed, including the following: increase or decrease in blood potassium, increase in blood creatinine, increase in blood uric acid, increase liver function tests (gamma glutamyl transferase levels).
Rare (affects less than 1 in 1000 patients):
Hypersensitivity to the drug; fainting; redness and warmth of the face; rash with hives; swelling of the face.
Side effects reported with use of olmesartan medoxomil or amlodipine alone, but not with Bivis or more frequently:
Olmesartan medoxomil
Common (affects less than 1 in 10 patients):
Bronchitis; sore throat; stuffy or runny nose; cough; abdominal pain; gastrointestinal flu; diarrhea; indigestion; nausea; pain in the bones or joints; back pain; blood in the urine; urinary tract infection; chest pain; flu-like symptoms; ache. Changes in laboratory tests such as increased fat (hypertriglyceridaemia); increase in plasma urea or uric acid and increase in liver and muscle function tests.
Uncommon (affects less than 1 in 100 patients):
Reduction in the number of a type of blood cell called platelets, which can make bruising easier or prolong bleeding time immediate allergic reactions that can affect the whole body and can cause breathing problems or a rapid drop in blood pressure which can also lead to weakness (anaphylactic reactions); angina (pain or discomfort in the chest, known as angina pectoris); itching; rash rash; allergic rash; rash with hives, swelling of the face; muscle pain; feeling sick.
Rare (affects less than 1 in 1000 patients):
Swelling of the face, mouth and / or larynx (seat of the vocal cords); acute renal failure and renal failure; lethargy.
Amlodipine
Common (affects less than 1 in 10 patients):
Abdominal pain; nausea; swollen ankles; drowsiness; redness and warmth of the face.
Uncommon (affects less than 1 in 100 patients):
Restless sleep; sleep disorders; mood disorders including anxiety; depression; irritability; tremors; changes in taste; fainting; visual disturbances including double vision; ringing in the ears (tinnitus); worsening of angina pectoris (chest pain or discomfort); stuffy or runny nose; hair loss; red spots or spots on the skin due to small bleeding (purpura); skin discoloration; excessive sweating; rash; itching ; pain in muscles or joints; problems with urination; need to urinate at night; increased need to urinate; enlargement of breasts in men; chest pain; pain, malaise; weight gain or loss.
Rare (affects less than 1 in 1000 patients):
Confusion
Very rare (affects less than 1 in 10,000 patients):
Reduction in the number of white blood cells in the blood, which can increase the risk of infections reduction in the number of a type of blood cell called platelets, which may make bruising easier or prolong bleeding time; increased blood glucose; increased muscle stiffness or increased resistance to passive movements (hypertonia); tingling or numbness in the hands or feet; heart attack and irregular heartbeat; inflammation of blood vessels; inflammation of the liver or pancreas; inflammation of the stomach wall; thickening of the gums; elevated liver enzyme levels; yellowing of the skin and eyes; increased sensitivity of the skin to light; allergic reactions (itching, rash, swelling of the face, mouth and / or larynx (location of the vocal cords) along with itching and rash, other allergic conditions with inflammation and peeling of the skin, sometimes life threatening).
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the national reporting system at https://www.aifa.gov.it/content/segnalazioni-reazioni-avverse. By reporting side effects you can help provide more information on safety. of this medicine.
Expiry and Retention
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the carton. The expiry date refers to the last day of the month.
This medicine does not require any special storage conditions.
Do not throw any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. This will help protect the environment.
What Bivis contains
The active substances are olmesartan medoxomil and amlodipine (as besylate).
Each film-coated tablet contains 20 mg of olmesartan medoxomil and 5 mg of amlodipine (as besylate).
Each film-coated tablet contains 40 mg of olmesartan medoxomil and 5 mg of amlodipine (as besylate).
Each film-coated tablet contains 40 mg of olmesartan medoxomil and 10 mg of amlodipine (as besylate).
The excipients are
Tablet core: pregelatinised maize starch, silicified microcrystalline cellulose, croscarmellose sodium, magnesium stearate.
Coating: polyvinyl alcohol, macrogol 3350, talc, titanium dioxide (E171) and iron (III) oxide (E172, Bivis 40 mg / 5 mg and 40 mg / 10 mg film-coated tablets only).
Description of what Bivis looks like and contents of the pack
Bivis 20 mg / 5 mg, white, round, film-coated tablets, debossed with C73 on one side;
Bivis 40 mg / 5 mg, cream-colored, round, film-coated tablets debossed with C75 on one side;
Bivis 40 mg / 10 mg, round, brownish film-coated tablets, debossed with C77 on one side.
Bivis is available in packs of 14, 28, 30, 56, 90, 98, 10x28 and 10x30 film-coated tablets, and in packs of 10, 50 and 500 film-coated tablets with perforated unit dose blisters.
Not all pack sizes may be marketed.
Source Package Leaflet: AIFA (Italian Medicines Agency). Content published in January 2016. The information present may not be up-to-date.
To have access to the most up-to-date version, it is advisable to access the AIFA (Italian Medicines Agency) website. Disclaimer and useful information.
01.0 NAME OF THE MEDICINAL PRODUCT
BIVIS TABLETS COATED WITH FILM
02.0 QUALITATIVE AND QUANTITATIVE COMPOSITION
Bivis 20 mg / 5 mg film-coated tablets:
Each Bivis film-coated tablet contains 20 mg of olmesartan medoxomil and 5 mg of amlodipine (as amlodipine besylate).
Bivis 40 mg / 5 mg film-coated tablets:
Each Bivis film-coated tablet contains 40 mg of olmesartan medoxomil and 5 mg of amlodipine (as amlodipine besylate).
Bivis 40 mg / 10 mg film-coated tablets:
Each Bivis film-coated tablet contains 40 mg of olmesartan medoxomil and 10 mg of amlodipine (as amlodipine besylate).
For the full list of excipients, see section 6.1
03.0 PHARMACEUTICAL FORM
Film-coated tablet.
Bivis 20 mg / 5 mg film-coated tablets: White, 6 mm round, film-coated tablets with C73 on one side.
Bivis 40 mg / 5 mg film-coated tablets: cream colored, round shaped film-coated tablets of 8 mm with C75 debossed on one side
Bivis 40 mg / 10 mg film-coated tablets: brownish, round, 8 mm film-coated tablets with C77 on one side.
04.0 CLINICAL INFORMATION
04.1 Therapeutic indications
Treatment of essential arterial hypertension.
Bivis is indicated in adult patients whose blood pressure is not adequately controlled by olmesartan medoxomil or amlodipine alone (see sections 4.2 and 5.1).
04.2 Posology and method of administration
Dosage:
Adults
The recommended dose of Bivis is one tablet per day.
Bivis 20 mg / 5 mg can be administered in those patients whose blood pressure is not adequately controlled by therapy with 20 mg olmesartan medoxomil or 5 mg amlodipine alone.
Bivis 40 mg / 5 mg can be administered in those patients whose blood pressure is not adequately controlled by Bivis 20 mg / 5 mg therapy.
Bivis 40 mg / 10 mg can be administered in those patients whose blood pressure is not adequately controlled by Bivis 40 mg / 5 mg therapy.
Before switching to the fixed combination, it is recommended to increase the dosage of the individual components. A direct switch from monotherapy to fixed combination can be considered when clinically appropriate.
Patients receiving olmesartan medoxomil and amlodipine as separate tablets can be switched to Bivis tablets for convenience, containing the same doses as the active substances.
Bivis can be taken regardless of food.
Older people (65 years or older)
Dosage adjustments are not generally required in older people, but dose escalation should be considered with caution (see sections 4.4 and 5.2). If the maximum daily dose of 40 mg olmesartan medoxomil is required, blood pressure should be carefully considered. monitored.
Altered kidney function
The maximum dose of olmesartan medoxomil in patients with mild or moderate renal impairment (creatinine clearance between 20 and 60 ml / min) is 20 mg olmesartan medoxomil once daily due to limited clinical experience with higher doses in this patient group. The use of Bivis in patients with severe renal impairment (creatinine clearance less than 20 ml / min) is not recommended (see sections 4.4 and 5.2). Monitoring of potassium and potassium levels is recommended in patients with moderate renal impairment. of creatinine.
Altered liver function
Bivis should be used with caution in patients with mild or moderate hepatic impairment (see sections 4.4 and 5.2).
In patients with moderate hepatic impairment, a starting dose of 10 mg olmesartan medoxomil once daily is recommended and the maximum dose should not exceed 20 mg once daily. In patients with hepatic impairment taking diuretics and / or other antihypertensive drugs, careful monitoring of blood pressure and renal function is advised. There is no experience of the use of olmesartan medoxomil in patients with severe hepatic impairment.
As with all calcium channel blockers, in patients with impaired hepatic function, the half-life of amlodipine is prolonged and dosage recommendations have not been established. Therefore, Bivis should be administered with caution in these patients. The pharmacokinetics of amlodipine have not been studied in severe hepatic impairment. In patients with severe hepatic impairment, treatment with amlodipine should be initiated at the lowest dose followed by gradual dosage adjustment.The use of Bivis in patients with severe hepatic impairment is contraindicated (see section 4.3).
Pediatric population
The safety and efficacy of Bivis in children and adolescents below 18 years have not been established. No data available.
Method of administration:
The tablets should be swallowed with a sufficient amount of liquid (eg a glass of water). The tablets should not be chewed and should be taken at the same time each day.
04.3 Contraindications
Hypersensitivity to the active substances, to dihydropyridine derivatives or to any of the excipients listed in section 6.1.
Second and third trimester of pregnancy (see sections 4.4 and 4.6).
Severe hepatic insufficiency and biliary obstruction (see section 5.2).
The concomitant use of Bivis with aliskiren-containing products is contraindicated in patients with diabetes mellitus or renal impairment (GFR 2) (see sections 4.5 and 5.1).
Due to the amlodipine contained, Bivis is also contraindicated in patients with:
- severe hypotension
- shock (including cardiogenic shock)
- obstruction of the outflow tract of the left ventricle (e.g. high grade aortic stenosis)
- haemodynamically unstable heart failure after acute myocardial infarction
04.4 Special warnings and appropriate precautions for use
Patients with hypovolaemia or sodium depletion:
In patients with hypovolaemia and / or sodium depletion caused by high doses of diuretics, reduced dietary sodium intake, diarrhea or vomiting, symptomatic hypotension may occur, especially after the first dose. These conditions must be corrected, or close medical supervision is required, before starting treatment with Bivis.
Other conditions related to stimulation of the renin-angiotensin-aldosterone system:
In patients whose vascular tone and kidney function are primarily dependent on the activity of the renin-angiotensin-aldosterone system (eg, patients with severe congestive heart failure or kidney disease, including renal artery stenosis), treatment with drugs that affect this system, such as angiotensin II receptor antagonists, has been associated with acute hypotension, azotemia, oliguria or, rarely, acute renal failure.
Renovascular hypertension:
In patients with bilateral renal artery stenosis, or stenosis of the afferent artery to a single functioning kidney, treated with drugs that affect the renin-angiotensin-aldosterone system, there is an increased risk of renal failure and severe hypotension.
Altered kidney function and kidney transplant:
When Bivis is used in patients with impaired renal function, it is recommended that serum potassium and creatinine levels be checked periodically. Bivis must not be used in patients with severe renal impairment (creatinine clearance less than 20 ml / min) (see sections 4.2 and 5.2). There is no experience with the administration of Bivis in patients with recent kidney transplantation or in patients with end stage renal insufficiency (creatinine clearance less than 12 ml / min).
Dual blockade of the renin-angiotensin-aldosterone system (RAAS):
There is evidence that concomitant use of ACE inhibitors, angiotensin II receptor blockers or aliskiren increases the risk of hypotension, hyperkalaemia and decreased renal function (including acute renal failure). Dual blockade of the RAAS through the combined use of ACE inhibitors, angiotensin II receptor blockers or aliskiren is therefore not recommended (see sections 4.5 and 5.1).
If dual block therapy is considered absolutely necessary, this should only be done under the supervision of a specialist and with close and frequent monitoring of kidney function, electrolytes and blood pressure.
ACE inhibitors and angiotensin II receptor antagonists should not be used concomitantly in patients with diabetic nephropathy.
Impaired liver function:
Exposure to amlodipine and olmesartan medoxomil is increased in patients with hepatic impairment (see section 5.2). Bivis should be administered with caution in patients with mild or moderate hepatic impairment. In patients with moderate impairment, the dose of olmesartan medoxomil should not exceed 20 mg (see section 4.2). In patients with impaired hepatic function, amlodipine should therefore initially be taken at the lowest dose and used with caution both at initiation of treatment and when increasing the dose. Bivis is contraindicated in patients with severe hepatic impairment (see section 4.3).
Hyperkalaemia:
As with other angiotensin II antagonists and ACE inhibitors, hyperkalaemia may occur during treatment, especially in the presence of renal impairment and / or heart failure (see section 4.5). Close monitoring of serum potassium is recommended in patients at risk. . Concomitant use of potassium supplements, potassium-sparing diuretics, potassium-containing salt substitutes, or other medicinal products that may induce elevations of potassium levels (such as heparin) should be done with caution with frequent monitoring of potassium levels. potassium.
Lithium:
As with other angiotensin II receptor antagonists, concomitant administration of lithium and Bivis is not recommended (see section 4.5).
Aortic or mitral valve stenosis, obstructive hypertrophic cardiomyopathy:
Due to the presence of amlodipine in Bivis, as with all other vasodilators, particular caution is recommended in patients suffering from aortic or mitral valve stenosis or obstructive hypertrophic cardiomyopathy.
Primary aldosteronism:
Patients with primary aldosteronism generally do not respond to antihypertensive drugs acting by inhibition of the renin-angiotensin system. Therefore, the use of Bivis is not recommended in these patients.
Heart failure:
As a consequence of inhibition of the renin-angiotensin-aldosterone system, changes in renal function may be expected in susceptible individuals. In patients with severe heart failure whose renal function may be dependent on the activity of the renin-angiotensin-aldosterone system, treatment with angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor antagonists has been associated with oliguria and / or progressive azotemia and (rarely) with acute renal failure and / or death.
Patients with heart failure should be treated with caution. In a long-term, placebo-controlled study of amlodipine in patients with severe heart failure (NYHA class III and IV), the reported incidence of pulmonary edema was higher in the amlodipine group than in the placebo group (see section 5.1). Calcium channel blockers, including amlodipine, should be used with caution in patients with congestive heart failure, as they may increase the risk of future cardiovascular events and mortality.
Sprue-like enteropathy:
In very rare cases, chronic diarrhea with significant weight loss, possibly caused by a delayed localized hypersensitivity reaction, has been reported in patients receiving olmesartan for a few months or years. Intestinal biopsies from patients often revealed villous atrophy. If a patient experiences these symptoms during treatment with olmesartan other etiologies should be excluded. Discontinuation of olmesartan medoxomil should be considered in cases where no "other etiology is identified."
In cases where symptoms disappear and sprue-like enteroparia is confirmed by a biopsy, treatment with olmesartan medoxomil should not be restarted.
Ethnic differences:
As with all other angiotensin II antagonists, the antihypertensive effect of Bivis may be less in black patients, possibly due to the higher prevalence of low renin levels in the black hypertensive population.
Older people:
Dosage increases should be done with caution in the elderly (see section 5.2).
Pregnancy:
Treatment with angiotensin II antagonists should not be initiated in pregnancy. Unless continued treatment with angiotensin II antagonists is considered essential, it should be replaced by an alternative antihypertensive treatment in patients planning pregnancy. has a recognized safety profile in pregnancy. When pregnancy is diagnosed, treatment with angiotensin II antagonists should be stopped immediately and, if deemed appropriate, alternative therapy should be started (see sections 4.3 and 4.6).
Other:
As with any other antihypertensive drug, excessive reduction in blood pressure in patients with ischemic heart disease or ischemic cerebrovascular disease can lead to myocardial infarction or stroke.
04.5 Interactions with other medicinal products and other forms of interaction
Potential interactions with the Bivis association:
Concomitant use requiring caution
Other antihypertensive drugs:
The hypotensive effect caused by Bivis may be increased by the concomitant use of other antihypertensive drugs (eg alpha blockers, diuretics).
Potential interactions with olmesartan medoxomil contained in Bivis:
Concomitant use not recommended
ACE inhibitors, angiotensin II receptor antagonists or aliskiren
Clinical trial data have shown that dual blockade of the renin-angiotensin-aldosterone system (RAAS) through the combined use of ACE inhibitors, angiotensin II receptor blockers or aliskiren is associated with a higher frequency of adverse events. such as hypotension, hyperkalaemia and decreased renal function (including acute renal failure) compared to the use of a single agent active on the RAAS system (see sections 4.3, 4.4 and 5.1).
Drugs that affect potassium levels:
The concomitant use of potassium-sparing diuretics, potassium supplements, potassium-containing salt substitutes or other drugs capable of increasing serum potassium levels (eg heparin, ACE inhibitors) may cause an increase in serum potassium. Serum potassium (see section 4.4) If drugs capable of affecting potassium levels are prescribed in combination with Bivis, monitoring of plasma potassium levels is recommended.
Lithium:
Reversible increases in serum lithium concentrations and toxicity have been reported during concomitant administration of lithium with angiotensin converting enzyme inhibitors and, rarely, with angiotensin II antagonists. combination lithium is not recommended (see section 4.4). If concomitant use is deemed necessary, careful monitoring of serum lithium levels is recommended.
Concomitant use requiring caution
Non-steroidal anti-inflammatory drugs (NSAIDs), including selective COX-2 inhibitors, acetylsalicylic acid (> 3 g / day) and non-selective NSAIDs:
When angiotensin II antagonists are administered concomitantly with NSAIDs, attenuation of the antihypertensive effect may occur. Furthermore, concomitant use of angiotensin II antagonists and NSAIDs may increase the risk of worsening of renal function and lead to an increase in serum potassium. Therefore, monitoring of renal function at the initiation of such concomitant treatment and adequate hydration of patients are recommended.
Colesevelam, bile acid sequestering agent
Concomitant administration of the bile acid sequestering colesevelam hydrochloride reduces the systemic exposure, maximum plasma concentration and t1 / 2 of olmesartan. Administration of olmesartan medoxomil at least 4 hours prior to colesevelam hydrochloride reduces the effect of this drug interaction . Administration of olmesartan medoxomil at least 4 hours prior to the colesevelam hydrochloride dose should be considered (see section 5.2).
Additional information:
A modest reduction in the bioavailability of olmesartan was observed after treatment with antacids (aluminum magnesium hydroxide).
Olmesartan medoxomil has no significant effect on the pharmacokinetics or pharmacodynamics of warfarin or the pharmacokinetics of digoxin.
Concomitant administration of olmesartan medoxomil and pravastatin did not cause clinically relevant effects on the pharmacokinetics of the two substances in healthy subjects.
Olmesartan has no clinically relevant inhibitory effects on human cytochrome P450 enzymes 1A1 / 2, 2A6, 2C8 / 9, 2C19, 2D6, 2E1 and 3A4 in vitro, while induction effects on rat cytochrome P450 are minimal or absent. Clinically relevant interactions between olmesartan and drugs metabolised by the aforementioned cytochrome P450 enzymes are not to be expected.
Potential interactions with amlodipine contained in Bivis:
Effects of other medicinal products on amlodipine
CYP3A4 inhibitors:
Concomitant use of amlodipine with potent or moderate CYP3A4 inhibitors (protease inhibitors, azole antifungals, macrolides such as erythromycin or clarithromycin, verapamil or diltiazem) may cause a significant increase in amlodipine exposure. The clinical significance of these pharmacokinetic changes. it may be more pronounced in older people, therefore clinical monitoring and dosage adjustment may be required.
CYP3A4 inducers
There are no data available on the effect of CYP3A4 inducers on amlodipine. Concomitant use of CYP3A4 inducers (eg rifampicin, Hypericum perforatum) may lead to lower plasma concentrations of amlodipine. Amlodipine should be used with caution together with CYP3A4 inducers.
Administration of amlodipine with grapefruit or grapefruit juice is not recommended as the bioavailability of amlodipine may increase and consequently potentiate the antihypertensive effect of amlodipine in some patients.
Dantrolene (infusion): Lethal ventricular fibrillation and cardiovascular collapse associated with hyperkalaemia have been observed in animals following intravenous administration of verapamil and dantrolene. Due to the risk of hyperkalaemia, it is recommended to avoid concomitant administration of calcium channel blockers such as amlodipine in patients prone to malignant hyperthermia and in the treatment of malignant hyperthermia.
Effects of amlodipine on other medicinal products
The hypotensive effects of amlodipine add to the hypotensive effects of other antihypertensive drugs.
In clinical interaction studies, amlodipine did not affect the pharmacokinetics of atorvastatin, digoxin, warfarin or cyclosporine.
Simvastatin: Co-administration of repeated doses of 10 mg of amlodipine with simvastatin 80 mg resulted in a 77% increase in exposure to simvastatin compared to simvastatin alone. Limit the dose of simvastatin to 20 mg daily in patients treated with amlodipine.
04.6 Pregnancy and lactation
Pregnancy (see section 4.3)
There are no data on the use of Bivis in pregnant patients. Animal reproductive toxicity studies have not been performed with Bivis.
Olmesartan medoxomil (active ingredient by Bivis)
The use of angiotensin II antagonists is not recommended in the first trimester of pregnancy (see section 4.4). The use of angiotensin II antagonists is contraindicated during the second and third trimesters of pregnancy (see sections 4.3 and 4.4).
Epidemiological data on the risk of teratogenicity following exposure to ACE inhibitors during the first trimester of pregnancy have not led to conclusive results; however, a small increase in risk cannot be excluded. Although there are no controlled epidemiological data on the risk with drug antagonists. "angiotensin II, a similar risk may exist for this class of drugs. Unless continued treatment with angiotensin II antagonists is considered essential, in patients planning pregnancy it should be replaced by an alternative antihypertensive treatment with a recognized safety profile in pregnancy. pregnancy, treatment with angiotensin II antagonists should be stopped immediately and, if deemed appropriate, alternative therapy should be started.
Exposure to angiotensin II antagonists during the second and third trimesters is known to induce fetal toxicity (decreased renal function, oligohydramnios, skull ossification retardation) and neonatal toxicity (renal failure, hypotension, hyperkalaemia) in women ( see paragraph 5.3).
Should exposure to angiotensin II antagonists have occurred from the second trimester of pregnancy onwards, ultrasound check of renal function and skull is recommended. Neonates whose mothers have taken angiotensin II antagonists should be closely monitored for hypotension (see sections 4.3 and 4.4).
Amlodipine (active ingredient by Bivis)
Data on a limited number of pregnancies with exposure to amlodipine do not indicate that amlodipine or other calcium channel blockers have a harmful effect on the health of the fetus.However, there may be a risk of prolonged labor.
Consequently, Bivis is not recommended during the first trimester of pregnancy and is contraindicated during the second and third trimesters of pregnancy (see sections 4.3 and 4.4).
Feeding time
Olmesartan is excreted in the breast milk of rats. However, it is not known whether the same occurs in human milk. It is not known whether amlodipine is excreted in milk. Calcium antagonists dihydropyridine, similar to amlodipine, are excreted in human milk. Since no data are available regarding the use of olmesartan and amlodipine during breastfeeding, Bivis is not recommended and alternative treatments with a proven safety profile are preferred for the use during lactation, especially in case of breastfeeding of newborns and premature babies.
Fertility
Reversible biochemical changes in the head of spermatozoa have been reported in patients treated with calcium channel blockers. There are insufficient clinical data on the potential effect of amlodipine on fertility. In a rat study, undesirable effects on male fertility were reported (see section 5.3).
04.7 Effects on ability to drive and use machines
Bivis has mild or moderate effects on the ability to drive and use machines. Dizziness, headache, nausea or symptoms of fatigue may occasionally occur in patients on antihypertensive therapy and may impair the ability to react. Caution is recommended especially at the start of treatment.
04.8 Undesirable effects
Bivis:
The most commonly reported adverse reactions during treatment with Bivis are peripheral edema (11.3%), headache (5.3%) and dizziness (4.5%).
Adverse reactions caused by Bivis in clinical trials, post-authorization safety studies and spontaneous reporting, as well as adverse reactions caused by the individual components olmesartan medoxomil and amlodipine based on the known safety profile of these substances are summarized in the table below.
To classify the frequency of occurrence of adverse reactions, the following terminology was used:
Very common (≥1 / 10);
Common (≥1 / 100,
Uncommon (≥1 / 1000,
Rare (≥1 / 10,000,
Very rare (
Single cases of rhabdomyolysis have been reported in temporal association with the intake of angiotensin II receptor blockers. Single cases of extrapyramidal syndrome have been reported in patients treated with amlodipine.
Reporting of suspected adverse reactions
Reporting of suspected adverse reactions occurring after authorization of the medicinal product is important as it allows continuous monitoring of the benefit / risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system. "address www.agenziafarmaco.gov.it/it/responsabili.
04.9 Overdose
Symptoms:
There is no experience of overdose of Bivis. The most likely effects of olmesartan medoxomil overdose are hypotension and tachycardia; bradycardia may occur if parasympathetic (vagal) stimulation occurs. Amlodipine overdose is likely to lead to excessive peripheral vasodilation with marked and possible hypotension. reflex tachycardia Marked and potentially prolonged systemic hypotension up to the onset of shock with fatal outcome has been reported.
Treatment:
Gastric lavage should be considered if intake is recent. Administration of activated charcoal immediately or within two hours of ingestion of amlodipine has been shown to substantially reduce the absorption of amlodipine in healthy subjects.
Clinically significant hypotension due to an overdose of Bivis requires active support of the cardiovascular system, including careful monitoring of cardiopulmonary function, elevation of extremities, and control of circulatory volume and urinary excretion. A vasoconstrictor can help restore vascular tone and blood pressure, as long as there are no contraindications to its use. Intravenous calcium gluconate may be useful in counteracting the calcium channel blocking effect.
Since amlodipine is highly bound to plasma proteins, dialysis is not expected to help. The dialysability of olmesartan is unknown.
05.0 PHARMACOLOGICAL PROPERTIES
05.1 Pharmacodynamic properties
Pharmacotherapeutic group: angiotensin II antagonists and calcium channel blockers.
ATC code: C09DB02.
Mechanism of action
Bivis is a combination of an angiotensin II receptor antagonist, olmesartan medoxomil, and a calcium antagonist, amlodipine besylate. The combination of these substances has an additive antihypertensive effect, reducing blood pressure to a greater degree than either component alone.
Clinical efficacy and safety
Bivis
In an 8-week, double-blind, randomized, placebo-controlled, factorial-design study in 1940 patients (71% Caucasian and 29% non-Caucasian), treatment with all doses of Bivis resulted in a reduction significantly higher systolic and diastolic blood pressure than monotherapy components. The mean change in systolic / diastolic blood pressure was dose dependent: -24 / -14 mmHg (combination 20 mg / 5 mg), -25 / -16 mmHg (combination 40 mg / 5 mg) and -30 / -19 mmHg ( combination 40 mg / 10 mg).
Bivis 40 mg / 5 mg reduced systolic / diastolic blood pressure in a sitting position by an additional 2.5 / 1.7 mmHg compared to Bivis 20 mg / 5 mg. Similarly, Bivis 40 mg / 10 mg reduced systolic / diastolic blood pressure in a sitting position by an additional 4.7 / 3.5 mmHg compared to Bivis 40 mg / 5 mg.
The percentage of patients who achieved blood pressure target (diabetics and diabetic patients) was 42.5%; 51.0%; and 49.1%; for Bivis 20 mg / 5 mg; 40 mg / 5 mg, respectively. and 40 mg / 10 mg.
Most of the antihypertensive effects of Bivis were generally achieved within the first two weeks of therapy.
A second randomized, double-blind, placebo-controlled study evaluated the efficacy of adding amlodipine to treatment in Caucasian patients whose blood pressure was inadequately controlled after eight weeks of treatment with 20 mg olmesartan medoxomil alone.
In patients who continued to receive 20 mg olmesartan medoxomil alone, systolic / diastolic blood pressure decreased by -10.6 / -7.8 mmHg after an additional eight weeks. Addition of 5 mg amlodipine for eight weeks resulted in a reduction in blood pressure. arterial systolic / diastolic blood of -16.2 / -10.6 mmHg (p = 0.0006).
The proportion of patients who achieved their blood pressure goal (
A further study evaluated the addition of different dosages of olmesartan medoxomil in Caucasian patients whose blood pressure was inadequately controlled after eight weeks of treatment with amlodipine 5 mg alone.
In patients who continued to receive 5 mg amlodipine alone, systolic / diastolic blood pressure decreased by -9.9 / -5.7 mmHg after an additional eight weeks. The addition of 20 mg olmesartan medoxomil resulted in a reduction in systolic / diastolic blood pressure of -15.3 / -9.3 mmHg and the addition of 40 mg olmesartan medoxomil resulted in a reduction in systolic / diastolic blood pressure of -16.7 / -9.5 mmHg (p
The proportion of patients who achieved their blood pressure goal (
No data are available from randomized studies in uncontrolled hypertensive patients, which have compared the use of a mean dose of Bivis combination treatment with escalating treatment with amlodipine or olmesartan alone.
The three studies performed confirmed that the hypotensive effect of Bivis once daily was maintained throughout the 24-hour dosing interval, with a trough-to-peak ratio of 71% to 82% for systolic and diastolic blood pressure. and with 24-hour efficacy confirmed by ambulatory blood pressure monitoring.
The antihypertensive efficacy of Bivis was similar regardless of age and gender, and was similar in patients with or without diabetes.
In two non-randomized, open-label extension studies, maintenance of the efficacy of Bivis 40 mg / 5 mg after one year was demonstrated in 49-67% of patients.
Olmesartan medoxomil (active ingredient of Bivis)
Olmesartan medoxomil, one of the active substances in Bivis is a selective angiotensin II type 1 receptor antagonist (type AT1). Olmesartan medoxomil is rapidly converted to its pharmacologically active metabolite, olmesartan. Angiotensin II is the major vasoactive hormone of the renin-angiotensin-aldosterone system and plays a significant role in the pathophysiology of hypertension. The effects of angiotensin II include vasoconstriction. , stimulation of aldosterone synthesis and release, cardiac stimulation and renal sodium reabsorption. Olmesartan blocks the vasoconstrictor and aldosterone-secreting effects of angiotensin II by blocking its binding to the AT1 receptor in tissues, including vascular smooth muscle and the adrenal gland. The action of olmesartan is independent of the origin or synthesis pathway of angiotensin II. The selective antagonism of olmesartan against the angiotensin II receptor (AT1) produces an increase in plasma levels renin and angiotensin I and II concentrations and some decrease in concentrations plasma actions of aldosterone.
In cases of hypertension, olmesartan medoxomil causes a dose-dependent, long-term reduction in blood pressure. sudden therapy.
Once-a-day administration of olmesartan medoxomil in hypertensive patients ensures an effective and constant reduction in blood pressure in the 24-hour interval between one dose and the next. For the same overall dosage, once-daily administration produced similar decreases in blood pressure. compared to administering the drug twice a day.
With continued treatment, maximum reduction in blood pressure is achieved within 8 weeks after initiation of therapy, although a substantial share of the blood pressure lowering effect is already observed after 2 weeks of treatment.
The effects of olmesartan on mortality and morbidity are currently unknown.
The Randomized Olmesartan and Diabetes Microalbuminuria Prevention (ROADMAP) study, conducted in 4,447 patients with type 2 diabetes, normoalbuminuria and at least one additional cardiovascular risk factor, investigated whether treatment with olmesartan could delay the onset of microalbuminuria. During the median follow-up period of 3.2 years, patients received olmesartan or placebo plus other antihypertensive drugs excluding ACE inhibitors or sartans.
The study demonstrated a significant risk reduction in terms of increased time to onset of microalbuminuria (primary endpoint) in favor of olmesartan. After adjustment for blood pressure values, this risk reduction was no longer statistically significant. 8.2% (178 out of 2160) of the patients in the olmesartan group and 9.8% (210 out of 2139) in the placebo group experienced microalbuminuria.
Regarding the secondary endpoints, cardiovascular events occurred in 96 patients (4.3%) in the olmesartan group and in 94 patients (4.2%) in the placebo group. The incidence of cardiovascular mortality was higher in the olmesartan group than in the placebo group (15 patients [0.7%] vs. 3 patients [0.1%]), despite similar values for non-fatal stroke (14 patients [0.6%] vs. . 8 patients [0.4%]), non-fatal myocardial infarction (17 patients [0.8%] vs. 26 patients [1.2%]) and non-cardiovascular mortality (11 patients [0.5%] vs. 12 patients [ 0.5%]). Overall mortality with olmesartan was numerically higher (26 patients [1.2%]) vs 15 patients [0.7%]) mainly due to a greater number of fatal cardiovascular events.
The Olmesartan Reducing Incidence of End-stage Renal Disease in Diabetic Nephropathy Trial (ORIENT) study evaluated the effects of olmesartan on renal and cardiovascular events in 577 Chinese and Japanese patients with type 2 diabetes and overt nephropathy. During the median follow-up period of 3.1 years, patients received olmesartan or placebo plus other antihypertensive drugs including ACE inhibitors.
The primary composite endpoint (time to first serum creatinine doubling event, end-stage nephropathy, death from all causes) occurred in 116 patients in the olmesartan group (41.1%) and 129 patients in the placebo group (45.4 %) (HR 0.97 [95% CI 0.75-1.24]; p = 0.791). The composite cardiovascular secondary endpoint occurred in 40 olmesartan-treated patients (14.2%) and 53 placebo-treated patients (18.7%). This composite cardiovascular endpoint included cardiovascular death in 10 patients (3.5%) receiving olmesartan versus 3. patients (1.1%) receiving placebo, total mortality 19 (6.7%) vs 20 (7.%), non-fatal stroke 8 (2.8%) vs 11 (3.9%) and non-fatal myocardial infarction 3 (1.1%) vs 7 (2.5%), respectively.
Amlodipine (active ingredient of Bivis)
Amlodipine, one of the active ingredients in Bivis, is a calcium channel antagonist that inhibits the transmembrane influx of calcium ions through L-type potential-dependent channels into the heart and smooth muscle. Experimental data indicate that amlodipine binds to both dihydropyridine and non-dihydropyridine binding sites. Amlodipine is relatively vessel selective, with a greater effect on smooth muscle cells than heart cells. The antihypertensive effect of amlodipine derives from a direct relaxing effect on arterial smooth muscle which leads to a reduction in peripheral resistance and, therefore, in blood pressure.
In hypertensive patients, amlodipine causes a dose-dependent, long-term decrease in blood pressure. therapy.
After administration of therapeutic doses to hypertensive patients, amlodipine causes a significant reduction in blood pressure in the supine, sitting and orthostatic position. Chronic use of amlodipine is not associated with significant changes in heart rate or plasma levels of catecholamines. In hypertensive patients with normal renal function, therapeutic doses of amlodipine reduce renal vascular resistance by increasing glomerular filtration rate and effective renal plasma flow, without changes in filtration fraction or proteinuria.
In haemodynamic studies conducted in patients with heart failure and in clinical trials based on exercise testing in patients with NYHA class II-IV heart failure, amlodipine did not cause any clinical deterioration, based on exercise tolerance, of left ventricular ejection fraction and clinical signs and symptoms.
A placebo-controlled study (PRAISE) aimed at evaluating patients with heart failure in NYHA class III-IV, who received digoxin, diuretics and ACE inhibitors, showed that amlodipine does not lead to an increased risk of mortality or risk. combined mortality and morbidity in patients with heart failure.
In a long-term, placebo-controlled (PRAISE-2) follow-up study of amlodipine in patients with NYHA Class III and IV heart failure, without clinical symptoms or objective findings suggestive of underlying ischemic disease, in treatment with stable doses of ACE inhibitors, digitalis and diuretics, amlodipine had no effect on cardiovascular or total mortality. In this same population, amlodipine was associated with increased reports of pulmonary edema although there was no significant difference in the incidence of worsening heart failure compared to placebo.
Heart Attack Prevention Treatment Study (ALLHAT)
A randomized double-blind morbidity-mortality study, called the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) was performed to compare the newer drug therapies: amlodipine 2.5-10 mg / day (calcium channel blocker ) or lisinopril 10-40 mg / day (ACE inhibitor) as first-line therapies, chlorthalidone 12.5-25 mg, thiazide diuretic, in mild to moderate hypertension. A total of 33,357 hypertensive patients of equal or equal age over 55 years were randomized and followed for a mean of 4.9 years. Patients had at least one additional risk factor for coronary artery disease, including: previous myocardial infarction or stroke (> 6 months prior to enrollment) or documentation of other atherosclerotic cardiovascular disease (overall 51.5%), type 2 diabetes (36.1%), HDL cholesterol left ventricular hypertrophy diagnosed on EKG or echocardiography (20.9%), cigarette smoker (2 1.9%). The primary end point was fatal coronary artery disease or non-fatal myocardial infarction. There was no significant difference in the primary end point between amlodipine and chlorthalidone based therapy: RR 0.98 95% CI ( 0.90-1.07) p = 0.65. Among the secondary endpoints, the incidence of heart failure (component of a composite cardiovascular composite endpoint) was significantly higher in the amlodipine group compared with the chlorthalidone group (10.2% vs. 7.7%, RR1, 38 95% CI [1.25-1.52] p
Other information:
Two large randomized controlled trials (ONTARGET (ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial) and VA Nephron-D (The Veterans Affairs Nephropathy in Diabetes)) have examined the use of the combination of an ACE inhibitor with an antagonist of the angiotensin II receptor.
ONTARGET was a study conducted in patients with a history of cardiovascular or cerebrovascular disease, or type 2 diabetes mellitus associated with evidence of organ damage. VA NEPHRON-D was a study conducted in patients with type 2 diabetes mellitus and diabetic nephropathy.
These studies did not demonstrate any significant beneficial effect on renal and / or cardiovascular outcomes and mortality, while an increased risk of hyperkalaemia, acute renal injury and / or hypotension was observed compared to monotherapy.
These results are also relevant for other ACE inhibitors and angiotensin II receptor antagonists, given their similar pharmacodynamic properties.
ACE inhibitors and angiotensin II receptor antagonists should therefore not be used simultaneously in patients with diabetic nephropathy.
ALTITUDE (Aliskiren Trial in Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints) was a study aimed at verifying the advantage of adding aliskiren to standard therapy of an ACE inhibitor or angiotensin II receptor antagonist in patients with diabetes mellitus. type 2 and chronic kidney disease, cardiovascular disease, or both. The study was terminated early due to an increased risk of adverse events. Cardiovascular death and stroke were both numerically more frequent in the aliskiren group than in the placebo group, and adverse events and serious adverse events of interest (hyperkalaemia, hypotension and renal dysfunction) were reported more frequently in the aliskiren group than in the placebo group.
05.2 Pharmacokinetic properties
Bivis
Following oral intake of Bivis, maximum plasma concentrations of olmesartan and amlodipine are reached after 1.5-2 hours and 6-8 hours, respectively. The speed of absorption and the amount absorbed of the two active substances of Bivis are equivalent to the speed and the amount following the intake of the two components as separate tablets. Food does not affect the bioavailability of olmesartan and amlodipine from Bivis.
Olmesartan medoxomil (active ingredient of Bivis)
Absorption and distribution
Olmesartan medoxomil is a pro-drug rapidly converted to a pharmacologically active metabolite, olmesartan, by esterases in the intestinal mucosa and portal circulation during absorption from the gastrointestinal tract. There is no trace of intact or side chain olmesartan medoxomil. intact medoxomil in plasma or excreta The mean absolute bioavailability of olmesartan, in the tablet formulation, was 25.6%.
The mean peak plasma concentration (Cmax) of diolmesartan is reached within approximately 2 hours of oral administration of olmesartan medoxomil; Plasma concentrations of olmesartan increase approximately linearly as the single oral dose increases to approximately 80 mg.
Food administration has minimal effects on the bioavailability of olmesartan and, therefore, olmesartan medoxomil can be administered in the fasted or fed state.
No clinically relevant differences in the pharmacokinetics of olmesartan dependent on patient sex were observed.
Olmesartan binds strongly to plasma proteins (99.7%), but the possibility of clinically significant protein binding displacement interactions between olmesartan and other highly bound active substances administered concurrently is low (as confirmed by the absence of a "clinically significant interaction between olmesartan medoxomil and warfarin). Blood cell binding of olmesartan is negligible. The mean volume of distribution after intravenous administration is low (16-29 L).
Biotransformation and elimination
Total plasma clearance of olmesartan was 1.3 L / h (CV, 19%), relatively low when compared to hepatic flux (approx. 90 L / h). After oral administration of a single dose of olmesartan medoxomil labeled with 14C, 10-16% of the administered radioactivity was excreted in the urine (largely within 24 hours after administration), while the remaining radioactivity was excreted in the faeces. Based on a systemic bioavailability of 25, 6%, it can be estimated that the absorbed olmesartan is eliminated by renal (approximately 40%) and hepatobiliary (approximately 60%) excretion. All recovered radioactivity was identified as olmesartan. No other significant metabolites were identified. The enterohepatic circle of olmesartan is minimal. Since a large amount of olmesartan is eliminated via the biliary route, use in patients with biliary obstruction is contraindicated (see section 4.3).
The terminal elimination half-life of olmesartan varies between 10 and 15 hours after repeated oral administration. Steady state was achieved after the first few administrations and no further accumulation was detected after 14 days of repeated administration. Renal clearance was approximately 0.5-0.7 L / h and was independent of dose.
Drug interactions
Colesevelam, bile acid sequestering agent
Concomitant administration of 40 mg olmesartan medoxomil and 3750 mg colesevelam hydrochloride to healthy subjects resulted in a 28% reduction in Cmax and 39% in AUC of olmesartan. Minor effects, 4% and 15% reduction, respectively, in Cmax and AUC were observed when olmesartan medoxomil was administered 4 hours prior to colesevelam hydrochloride. The elimination half-life of olmesartan was reduced by 50-52% regardless of concomitant administration or 4 hours prior to colesevelam hydrochloride (see section 4.5).
Amlodipine (active ingredient of Bivis)
Absorption and distribution
After oral administration of therapeutic doses, amlodipine is well absorbed, with peak plasma levels within 6-12 hours after administration. Absolute bioavailability has been estimated to be between 64 and 80%. The volume of distribution is approximately 21 L / kg. In vitro studies have shown that amlodipine binds approximately 97.5% to plasma proteins. food does not alter the bioavailability of amlodipine.
Biotransformation and elimination
The terminal plasma elimination half-life is approximately 35-50 hours, which justifies once-daily administration. Amlodipine is extensively metabolised by the liver to inactive compounds, 10% is eliminated in the urine as the base molecule and 60% in the metabolised form .
Olmesartan medoxomil and amlodipine (active ingredients of Bivis)
Special populations
Pediatric population (under 18 years of age):
No pharmacokinetic data are available in pediatric patients.
Older people (65 years or older):
In hypertensive patients, steady-state AUC of olmesartan was increased by approximately 35% in elderly people (65 to 75 years) and by approximately 44% in very elderly (3 75 years) compared to patients younger (see section 4.2). This may be related, at least in part, to a mean decrease in renal function in this patient group. The recommended dosing regimen in older people, however, is the same, although caution should be exercised in increasing the dosage.
The time to reach peak plasma concentrations of amlodipine is similar in young and elderly subjects. Amlodipine clearance tends to decrease in elderly persons resulting in increased AUC and elimination half-life. The increases in AUC and elimination half-life in patients with congestive heart failure were as expected for the age of the patient group involved in this study (see section 4.4).
Altered kidney function:
In patients with impaired renal function, steady-state AUC of olmesartan was increased by 62%, 82% and 179% in patients with mild, moderate and severe renal impairment, respectively, compared to healthy controls (see sections 4.2, 4.4 ).
Amlodipine is extensively metabolised to inactive metabolites. 10% of the substance is excreted unchanged in the urine. Changes in plasma concentrations of amlodipine are not correlated with the degree of renal impairment. In these patients, amlodipine can be administered at the normal dosage. Amlodipine is not dialysable.
Altered liver function:
After single oral administration, the AUC values of olmesartan were 6% and 65% higher, respectively, in patients with mild and moderate hepatic impairment compared to subjects with normal hepatic function. administration was 0.26% in healthy subjects, 0.34% in patients with mild hepatic impairment and 0.41% in those with moderate hepatic impairment. After repeated oral administration in patients with moderate hepatic impairment, values AUC of olmesartan was still 65% higher than in subjects with normal hepatic function. The mean C values of olmesartan are similar in patients with hepatic impairment and in healthy subjects. Olmesartan medoxomil has not been studied in patients with severe hepatic impairment (see sections 4.2, 4.4).
Very limited clinical data are available regarding the administration of amlodipine in patients with hepatic insufficiency. In patients with impaired hepatic function, the clearance of amlodipine is reduced and the half-life prolonged, resulting in an increase in AUC values of approximately 40% -60% (see sections 4.2, 4.4).
05.3 Preclinical safety data
Based on the non-clinical toxicity profile of each substance, no toxicity exacerbations of the combination are expected, since the two substances act on different targets: the kidney for olmesartan medoxomil and the heart for amlodipine.
In a repeat dose toxicity study of oral olmesartan medoxomil / amlodipine combination for three months in rats, the following changes were observed: decreased red blood cell count related parameters and renal changes, both referable to olmesartan; intestinal changes ( dilation of the lumen and diffuse thickening of the mucosa of the ileum and colon) adrenal (hypertrophy of the glomerular cortical cells and vacuolation of the fascicular cortical cells) and hypertrophy of the ducts of the mammary gland, referable to amlodipine. These alterations do not increase the existing and previously reported toxicity individually for the two active ingredients, nor do they lead to new toxicity, and no toxicologically synergistic effects have been observed.
Olmesartan medoxomil (active ingredient of Bivis)
In chronic toxicity studies in rats and dogs, olmesartan medoxomil has been shown to have similar effects to other AT1 receptor antagonists and ACE inhibitors: increased plasma urea (BUN) and creatinine; reduction in heart weight; reduction of erythrocyte parameters (erythrocytes, hemoglobin, hematocrit); histological indications of renal damage (regenerative lesions of the renal epithelium, thickening of the basement membrane, tubular dilatation). These adverse effects caused by the pharmacological actions of olmesartan medoxomil have also been observed in preclinical studies with other AT1 receptor antagonists and ACE inhibitors and may be reduced by the simultaneous oral administration of sodium chloride. Increased plasma renin activity and hypertrophy / hyperplasia of juxtaglomerular cells of the kidney have been observed in both species. These changes, which are a typical class effect of ACE inhibitors and AT1 receptor antagonists, appear to have no clinical relevance.
As with other AT1 receptor antagonists, olmesartan medoxomil has been shown to increase the incidence of chromosomal breaks in cell cultures in vitro. No relevant effects have been observed in numerous in vivo studies using olmesartan medoxomil at very high oral doses, up to 2000 mg / kg. Overall data from a comprehensive genotoxicity program suggest that olmesartan is very unlikely to exhibit any effects. genotoxic under conditions of clinical use.Olmesartan medoxomil did not show carcinogenicity in either a two-year study in rats or two six-month carcinogenicity studies in transgenic mice.
In reproductive studies in rats, olmesartan medoxomil did not affect fertility and there was no evidence of teratogenicity. In common with other angiotensin II antagonists, offspring survival was reduced after exposure to olmesartan medoxomil and was observed. dilation of the renal pelvis after exposure of mares during late pregnancy and lactation. In common with other antihypertensive agents, olmesartan medoxomil was shown to be more toxic in pregnant rabbits than in pregnant rats, however there was no indication. of foetotoxic effects.
Amlodipine (active ingredient of Bivis)
Reproductive toxicology
Reproduction studies in rats and mice have shown delayed parturition, prolonged labor and reduced neonatal survival at doses approximately 50 times the maximum recommended human dose based on the mg / kg ratio.
Reduction of fertility
There was no effect on the fertility of rats treated with amlodipine (males for 64 days and females for 14 days prior to mating) at doses up to 10 mg / kg / day (equivalent to 8 times the maximum dose of 10 mg on a recommended mg / m2 basis in humans *). Another study conducted in male rats treated with amlodipine besylate for 30 days at a dose comparable to that administered to humans (mg / kg), showed a decrease in testosterone and follicle-stimulating hormone in plasma, as well as decreases in density. sperm and the number of mature sperm cells and Sertoli cells.
Carcinogenesis, mutagenesis
Rats and mice treated for two years with dietary amlodipine, at concentrations calculated to provide daily levels of 0.5, 1.25 and 2.5 mg / kg / day, showed no evidence of carcinogenicity. The highest dose (for rats equal to twice the maximum clinical recommended dose of 10 mg on a mg / m2 basis in humans * and for mice similar to this maximum recommended dose) was close to the maximum tolerated dose for mice, but not from rats.
Mutagenicity studies did not reveal any drug-related effects on either the genetic or chromosomal level.
* Calculated on a patient weighing 50 kg.
06.0 PHARMACEUTICAL INFORMATION
06.1 Excipients
Core of the tablet
Pregelatinised maize starch
Silicified microcrystalline cellulose (microcrystalline cellulose with colloidal silicon dioxide)
Croscarmellose sodium
Magnesium stearate
Coating
Polyvinyl alcohol
Macrogol 3350
Talc
Titanium dioxide (E 171)
Iron (III) oxide yellow (E 172) (Bivis 40 mg / 5 mg and 40 mg / 10 mg film-coated tablets only)
Red iron (III) oxide (E 172) (Bivis 40 mg / 10 mg film-coated tablets only)
06.2 Incompatibility
Not relevant.
06.3 Period of validity
5 years.
06.4 Special precautions for storage
This medicine does not require any special storage conditions.
06.5 Nature of the immediate packaging and contents of the package
OPA / aluminum / PVC / aluminum blisters.
Packs contain 14, 28, 30, 56, 90, 98, 10X28 or 10x30 film-coated tablets. The perforated unit dose blister packs contain 10, 50 and 500 film-coated tablets.
Not all pack sizes may be marketed.
06.6 Instructions for use and handling
No special instructions.
07.0 MARKETING AUTHORIZATION HOLDER
MENARINI INTERNATIONAL Operations Luxembourg S.A.
1, Avenue de la Gare, L-1611 - Luxembourg
Dealer for sale: Laboratori Guidotti S.p.A. - Via Livornese 897, La Vettola - Pisa
08.0 MARKETING AUTHORIZATION NUMBER
BIVIS 20mg / 5mg film-coated tablets:
14 tablets AIC n. 038947014
28 tablets AIC n. 038947026
30 tablets AIC n. 038947038
56 tablets AIC n. 038947040
90 tablets AIC n. 038947053
98 tablets AIC n. 038947065
10x28 tablets AIC n. 038947077
10x30 tablets AIC n. 038947089
10 AIC tablets n. 038947091
50 tablets AIC n. 038947103
500 AIC tablets n. 038947115
BIVIS 40mg / 5mg film-coated tablets:
14 tablets AIC n. 038947127
28 tablets AIC n. 038947139
30 tablets AIC n. 038947141
56 tablets AIC n. 038947154
90 tablets AIC n. 038947166
98 tablets AIC n. 038947178
10x28 tablets AIC n. 038947180
10x30 tablets AIC n. 038947192
10 tablets AIC n. 038947204
50 tablets AIC n. 038947216
500 AIC tablets n. 038947228
BIVIS 40mg / 10mg film-coated tablets:
14 tablets AIC n. 038947230
28 tablets AIC n. 038947242
30 tablets AIC n. 038947255
56 tablets AIC n. 038947267
90 tablets AIC n. 038947279
98 tablets AIC n. 038947281
10x28 tablets AIC n. 038947293
10x30 tablets AIC n. 038947305
10 AIC tablets n. 038947317
50 tablets AIC n. 038947329
500 AIC tablets n. 038947331
09.0 DATE OF FIRST AUTHORIZATION OR RENEWAL OF THE AUTHORIZATION
Date of first authorization: 28 April 2009
Date of most recent renewal: July 12, 2013
10.0 DATE OF REVISION OF THE TEXT
April 2015