Active ingredients: Etoricoxib
ARCOXIA 30 mg film-coated tablets
ARCOXIA 60 mg film-coated tablets
ARCOXIA 90 mg film-coated tablets
ARCOXIA 120 mg film-coated tablets
Why is Arcoxia used? What is it for?
What is ARCOXIA and what is it for
- ARCOXIA belongs to a group of medicines called selective COX-2 inhibitors. These belong to a family of medicines known as non-steroidal anti-inflammatory drugs (NSAIDs).
- ARCOXIA helps reduce pain and swelling (inflammation) in the joints and muscles of people with osteoarthritis, rheumatoid arthritis, ankylosing spondylitis and gout.
- ARCOXIA is also used for the short-term treatment of moderate pain following dental surgery.
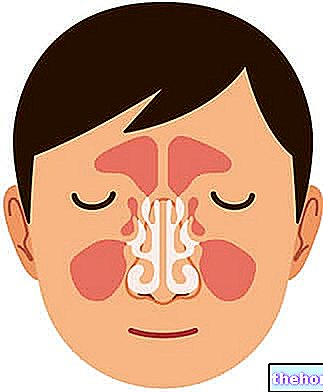
What is osteoarthritis (OA)?
Osteoarthritis is a disease of the joints. It is caused by the progressive deterioration of the cartilages that cover the ends of the bones. This leads to swelling (inflammation), pain, tenderness, stiffness and disability.
What is rheumatoid arthritis?
Rheumatoid arthritis is a long-term inflammatory joint disease. It causes pain, stiffness, swelling, and progressive loss of movement in affected joints. It can also cause inflammation in other parts of the body.
What is gout?
Gout is a disease with sudden and recurring bouts of very painful inflammation and redness of the joints. It is caused by the deposition of mineral crystals in the joints.
What is ankylosing spondylitis?
Ankylosing spondylitis is an inflammatory disease of the spine and large joints.
Contraindications When Arcoxia should not be used
Do not take ARCOXIA:
- if you are allergic (hypersensitive) to etoricoxib or any of the other ingredients of Arcoxia (see Further information, section 6)
- if you are allergic to non-steroidal anti-inflammatory drugs (NSAIDs), including aspirin and COX-2 inhibitors (see Possible Side Effects, section 4)
- if you have an active stomach ulcer or active stomach or bowel bleeding
- if you have severe liver disease
- if you have severe kidney disease
- if you are pregnant or there is a possibility that you are pregnant, or if you are breastfeeding (see "Pregnancy and breastfeeding")
- if you are under the age of 16
- if you have an inflammatory bowel disease such as Crohn's disease, ulcerative colitis, or colitis
- if your doctor has diagnosed you with heart problems such as heart failure (moderate or severe), angina (chest pain); or if you have had a heart attack; o if you have undergone coronary artery bypass surgery; if you have had "peripheral arterial disease (reduced circulation in the legs and feet due to narrowed or blocked blood vessels) or if you have had any type of stroke (including mini-stroke, transient ischemic attack or TIA)." etoricoxib may increase slightly the risk of heart attack and stroke; for this reason it should not be used in people who have already had heart problems or strokes
- if you have high blood pressure which is not controlled by treatment (ask your doctor or pharmacist if you are not sure if your blood pressure is under adequate control).
If you think any of these apply to you, do not take these tablets until you have consulted your doctor.
Precautions for use What you need to know before taking Arcoxia
Talk to your doctor or pharmacist before taking ARCOXIA if:
- Have a history of stomach bleeding or ulcers.
- You are dehydrated, for example due to a prolonged episode of vomiting or diarrhea.
- You have swelling due to fluid retention.
- Have a history of heart failure, or any other form of heart disease.
- Has a history of high blood pressure. In some people, ARCOXIA, especially at high doses, can increase blood pressure, and your doctor will periodically check your blood pressure.
- Have a history of liver or kidney disease.
- He is being treated for an "infection. ARCOXIA can mask or hide a fever, which is a sign of infection.
- She is a woman who is trying to get pregnant.
- He is an elderly person (over 65 years of age).
- You have diabetes, high cholesterol or a habit of smoking. These are conditions that can increase your risk of heart disease.
If you are unsure about any of the conditions just mentioned, talk to your doctor before taking ARCOXIA to check if the medicine is suitable for you.
ARCOXIA has the same efficacy in both the younger and the older patient. If you are elderly (over 65 years of age), your doctor will monitor you appropriately. No dose adjustment is necessary for elderly patients.
Children and adolescents
Do not give this medicine to children and adolescents under 16 years of age.
Interactions Which drugs or foods can modify the effect of Arcoxia
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, including those available without a doctor's prescription.
In particular, if you are taking any of the following medicines, your doctor may ask you to check whether these medicines are working well once you have started taking ARCOXIA:
- blood thinners (anticoagulants), such as warfarin
- rifampicin (an antibiotic)
- methotrexate (a drug used to suppress the immune system and often used in the treatment of rheumatoid arthritis)
- medicines used for high blood pressure and heart failure called ACE inhibitors and angiotensin receptor blockers, such as enalapril and ramipril, and losartan and valsartan
- lithium (a drug used for some types of depression)
- diuretics
- cyclosporine or tacrolimus (drugs used to suppress the immune system)
- digoxin (a medicine to treat heart failure and irregular heart rhythm)
- minoxidil (a drug to treat high blood pressure)
- salbutamol tablets or oral solution (a medicine to treat asthma)
- oral contraceptives
- hormone replacement therapy
- aspirin, the risk of stomach ulcers is higher if you take ARCOXIA with aspirin.
ARCOXIA can be taken with low doses of aspirin. If you are being treated with low-dose aspirin to prevent heart attack or stroke, you should not stop taking aspirin without consulting your doctor.
You should not take high doses of aspirin or anti-inflammatory medicines while taking ARCOXIA.
Warnings It is important to know that:
Pregnancy and breastfeeding
Arcoxia tablets should not be taken during pregnancy. If you are pregnant or suspected of pregnancy, or if you think you may become pregnant, do not take the tablets. If you become pregnant, stop taking the tablets and consult your doctor. If you are unsure or if you need more information about this, consult your doctor.
It is not known whether ARCOXIA is excreted in human milk. If you are breastfeeding, or think you will breastfeed, contact your doctor before taking ARCOXIA. If you are using ARCOXIA you must not breastfeed.
ARCOXIA with food and drink
The onset of the effect of ARCOXIA may be faster when taken without food.
Driving or using machines
Some patients taking ARCOXIA have reported dizziness and sleepiness.
Do not drive if you feel dizzy or sleepy.
Do not use tools or machines if you feel dizzy or sleepy.
ARCOXIA contains lactose
If you have been told by your doctor that you are unable to tolerate some sugars, contact your doctor before taking this drug.
Dose, Method and Time of Administration How to use Arcoxia: Posology
Always take this medicine exactly as your doctor has told you. If in doubt, consult your doctor or pharmacist.
Arcoxia tablets should not be taken by children or adolescents under 16 years of age.
Take ARCOXIA tablets once daily by mouth. ARCOXIA can be taken with or without food.
Do not take more than the recommended dose for the treatment of your disease. Your doctor will periodically evaluate your treatment. It is important that you use the lowest pain-control dose and that you do not take ARCOXIA for longer than necessary. This is because the risk of heart attacks and strokes can increase after prolonged treatment, especially with high doses.
Arthrosis
The recommended dose is 30 mg once daily, which can be increased to a maximum of 60 mg once daily if necessary.
Rheumatoid arthritis
The recommended dose is 90 mg once a day.
Ankylosing spondylitis
The recommended dose is 90 mg once a day.
Acute pain conditions
Etoricoxib should only be used for the acute painful period.
Gout
The recommended dose is 120 mg once daily which should only be used for the acute painful period, limited to a maximum of 8 days of treatment.
Postoperative pain from dental surgery
The recommended dose is 90 mg once daily, limited to a maximum of 3 days of treatment.
People with liver problems
- If you have mild liver disease you should not take more than 60 mg per day.
- If you have moderate liver disease, you should not take more than 30 mg per day.
Overdose What to do if you have taken too much Arcoxia
If you take more ARCOXIA than you should
You should never take more tablets than recommended by your doctor. If you take too many Arcoxia tablets you should contact a doctor immediately.
If you forget to take ARCOXIA
It is important to stick to the dose of ARCOXIA indicated by your doctor. If you forget a dose, just resume your usual dose schedule the next day. Do not take a double dose to make up for a forgotten tablet.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Side Effects What are the side effects of Arcoxia
Like all medicines, ARCOXIA can cause side effects, but they do not occur in all patients.
If any of the following symptoms occur, you should stop taking ARCOXIA and contact your doctor immediately:
- shortness of breath, chest pains, or swelling of the ankles that develop or start to get worse
- yellowing of the skin and eyes (jaundice) - these are symptoms of liver problems
- severe or continuous stomach pain or stools that turn black
- an allergic reaction which may include skin problems such as ulcers or blistering, or swelling of the face, lips, tongue, or throat which can make it difficult to breathe.
The frequency of possible side effects listed below is defined using the following convention:
Very common (affects more than 1 in 10 patients)
Common (affects 1 to 10 users in 100)
Uncommon (affects 1 to 10 users in 1,000)
Rare (affects 1 to 10 users in 10,000)
Very rare (affects less than 1 user in 10,000)
The following side effects may occur during treatment with ARCOXIA:
Very common:
- stomach pain
Common:
- alveolitis (inflammation and pain after a "tooth extraction)
- swelling of the legs and / or feet due to fluid retention (edema)
- dizziness, headache
- palpitations (fast or irregular heartbeat), irregular heart rhythm (arrhythmia)
- increased blood pressure
- wheezing or shortness of breath (bronchospasm)
- constipation, flatulence (excess gas), gastritis (inflammation of the inner surface of the stomach), heartburn, diarrhea, indigestion (dyspepsia) / stomach discomfort, nausea, retching (vomiting), inflammation of the esophagus, mouth ulcers
- changes in some blood tests related to liver function
- bruising
- weakness and fatigue, flu-like illness
Uncommon:
- gastroenteritis (inflammation of the gastrointestinal tract involving both the stomach and small intestine), upper respiratory infection, urinary tract infection
- decrease in the number of red blood cells, decrease in the number of white blood cells, decrease in platelets
- hypersensitivity (an allergic reaction including hives which may be severe enough to require immediate medical attention)
- increases or decreases in appetite, weight gain
- anxiety, depression, decreased mental acuity, visual, sensitive or auditory perceptions not caused by real stimuli (hallucinations)
- change in taste, difficulty sleeping, tingling or numbness, sleepiness
- blurred vision, irritation and redness of the eyes
- ringing in the ears, vertigo (persistent feeling of dizziness)
- abnormal heart rhythm (atrial fibrillation), rapid heart rate, heart failure, tightness, pressure or heaviness in the chest (angina pectoris), heart attack
- flushing, stroke, mini-stroke (transient ischemic attack), severe increase in blood pressure, inflammation of blood vessels
- cough, shortness of breath, nosebleeds
- bloating of the stomach or intestines, changes in bowel habits, dry mouth, stomach ulcer, inflammation of the inner surface of the stomach which can become severe and can lead to bleeding, irritable bowel syndrome, inflammation of the pancreas
- swelling of the face, skin rash or itchy skin, redness of the skin
- muscle cramps / spasms, muscle pain / stiffness
- high levels of potassium in the blood, changes in some blood or urine tests related to kidney function, severe kidney problems
- chest pain
Rare:
- angioedema (an allergic reaction with swelling of the face, lips, tongue and / or throat which may cause difficulty in breathing and swallowing, which may be severe enough to require immediate medical attention) / anaphylactic / anaphylactoid reactions including shock (a severe allergic reaction that requires immediate medical attention)
- confusion, restlessness
- liver problems (hepatitis)
- low levels of sodium in the blood
- liver failure, yellowing of the skin and / or eyes (jaundice)
- severe skin reactions
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
Expiry and Retention
Keep this medicine out of the sight and reach of children.
Do not take ARCOXIA after the expiry date indicated on the package. The expiry date refers to the last day of the month indicated.
Bottle: Keep the container tightly closed to protect the medicine from moisture.
Blisters: Store in the original package to protect the medicine from moisture.
Do not throw any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. This will help protect the environment.
Composition and pharmaceutical form
What ARCOXIA contains
- The active substance is etoricoxib. Each film-coated tablet contains 30, 60, 90 or 120 mg of etoricoxib.
- The other ingredients are: Inside of the tablets: anhydrous dibasic calcium phosphate, croscarmellose sodium, magnesium stearate, microcrystalline cellulose. Tablet coating: carnauba wax, lactose monohydrate, hypromellose, titanium dioxide (E171), triacetin. The 30, 60 and 120 mg tablets also contain yellow iron oxide (color E172) and indigo carmine (color E132).
What ARCOXIA looks like and what the package contains
ARCOXIA tablets are available in four formulations:
30 mg biconvex, apple-shaped, blue-green tablets, debossed with "ACX 30" on one side and "101" on the other;
60 mg, dark green, apple-shaped, biconvex tablets, debossed with "ARCOXIA 60" on one side and "200" on the other;
90 mg, biconvex, apple-shaped, white tablets debossed with "ARCOXIA 90" on one side and "202" on the other;
120 mg, biconvex, apple-shaped, light green tablets, debossed with "ARCOXIA 120" on one side and "204" on the other.
Packaging:
30 mg:
Packs of 2, 7, 14, 20, 28, 49 tablets or multi-packs of 98 (2 packs of 49) tablets in blisters.
60, 90 and 120 mg:
Packs of 2, 5, 7, 10, 14, 20, 28, 30, 50, 84, 100 tablets or multi-packs of 98 (2 packs of 49) tablets in blisters; or 30 and 90 tablets in bottles, with desiccant containers. The desiccant (one or two containers) in the bottle, used to keep the tablets dry, should not be swallowed.
Not all pack sizes may be marketed.
Source Package Leaflet: AIFA (Italian Medicines Agency). Content published in January 2016. The information present may not be up-to-date.
To have access to the most up-to-date version, it is advisable to access the AIFA (Italian Medicines Agency) website. Disclaimer and useful information.
01.0 NAME OF THE MEDICINAL PRODUCT
ARCOXIA
02.0 QUALITATIVE AND QUANTITATIVE COMPOSITION
Each film-coated tablet contains 30, 60, 90 or 120 mg of etoricoxib.
Excipients with known effects:
30 mg: lactose 1.3 mg
60 mg: lactose 2.7 mg
90 mg: lactose 4.0 mg
120 mg: lactose 5.3 mg
For the full list of excipients, see section 6.1.
03.0 PHARMACEUTICAL FORM
Film-coated tablets (tablets).
30 mg tablets: Green-blue, apple-shaped, biconvex tablets, debossed with "101" on one side and "ACX 30" on the other.
60 mg tablets: dark green, apple-shaped, biconvex tablets, debossed with "200" on one side and "ARCOXIA 60" on the other.
90 mg tablets: white, apple-shaped, biconvex tablets, debossed with "202" on one side and "ARCOXIA 90" on the other.
120 mg tablets: apple-shaped, light green biconvex tablets, debossed with "204" on one side and "ARCOXIA 120" on the other.
04.0 CLINICAL INFORMATION
04.1 Therapeutic indications
For the symptomatic treatment of osteoarthritis (OA), rheumatoid arthritis (RA), ankylosing spondylitis and the pain and signs of inflammation associated with acute gouty arthritis.
For the short-term treatment of moderate pain associated with dental surgery.
The decision to prescribe a selective COX-2 inhibitor should be based on an assessment of the individual patient's overall risks (see sections 4.3, 4.4).
04.2 Posology and method of administration
Dosage
Since the cardiovascular risks of etoricoxib may increase with dose and duration of exposure, the duration of treatment should be as short as possible and the lowest effective daily dose should be used. The need for treatment for symptomatic relief and response to therapy should be reassessed periodically, especially in patients with osteoarthritis (see sections 4.3, 4.4, 4.8 and 5.1).
Osteoarthritis
The recommended dose is 30 mg once daily. In some patients with insufficient symptom relief, increasing the dose to 60 mg once daily may increase efficacy. In the absence of increased therapeutic benefit, other therapeutic alternatives should be considered.
Rheumatoid arthritis
The recommended dose is 90 mg once daily.
Ankylosing spondylitis
The recommended dose is 90 mg once daily.
For acute pain conditions, etoricoxib should only be used during the acute symptom phase.
Acute gouty arthritis
The recommended dose is 120 mg once daily. In acute gouty arthritis clinical trials, etoricoxib was administered for 8 days.
Postoperative pain from dental surgery
The recommended dose is 90 mg once daily, limited to a maximum of 3 days. Some patients may need additional "postoperative analgesia."
Doses higher than those recommended for each indication have not shown greater efficacy or have not been studied. Consequentially:
The dose for OA should not exceed 60 mg / day.
The dose for RA and ankylosing spondylitis should not exceed 90 mg / day.
The dose for acute gouty arthritis should not exceed 120 mg / day, limited to a maximum of 8 days of treatment.
The dose for acute postoperative pain from dental surgery should not exceed 90 mg / day, limited to a maximum of 3 days.
Special populations
Senior citizens
No dose adjustments are required in the elderly. As with other drugs, caution should be exercised in elderly patients (see section 4.4).
Hepatic insufficiency
Regardless of indication, a dose of 60 mg once daily should not be exceeded in patients with mild hepatic dysfunction (Child-Pugh score 5-6). In patients with moderate hepatic dysfunction (Child-Pugh score 7-9), regardless of indication, a dose of 30 mg once daily should not be exceeded.
Clinical experience is particularly limited in patients with moderate hepatic dysfunction and caution should be exercised. There is no clinical experience in patients with severe hepatic dysfunction (Child-Pugh score ≥10); use of the drug is therefore contraindicated. in these patients (see sections 4.3, 4.4 and 5.2).
Kidney failure
No dose adjustment is required for patients with creatinine clearance ≥ 30 ml / min (see section 5.2). The use of etoricoxib in patients with creatinine clearance
Pediatric patients
Etoricoxib is contraindicated in children and adolescents below 16 years of age (see section 4.3).
Method of administration
ARCOXIA is administered orally and can be taken with or without food. The onset of effect of the medicinal product may be anticipated when ARCOXIA is administered between meals. This should be taken into account if rapid symptom relief is required.
04.3 Contraindications
Hypersensitivity to the active substance or to any excipient of this product listed in section 6.1.
Active peptic ulcer or active gastrointestinal (GI) bleeding.
Patients who have developed bronchospasm, acute rhinitis, nasal polyps, angioneurotic edema, urticaria or allergic-type reactions after taking acetylsalicylic acid or NSAIDs including COX-2 (cyclooxygenase-2) inhibitors.
Pregnancy and lactation (see sections 4.6 and 5.3).
Severe hepatic dysfunction (serum albumin
Estimated renal creatinine clearance
Children and adolescents under the age of 16.
Chronic inflammation of the intestine.
Congestive heart failure (NYHA II-IV).
Hypertensive patients in whom blood pressure is persistently above 140/90 mmHg and is not adequately controlled.
Established ischemic heart disease, peripheral arterial disease and / or cerebral vascular disease.
04.4 Special warnings and appropriate precautions for use
Gastrointestinal effects
Upper gastrointestinal complications [perforation, ulcers or bleeding (SUP)] have occurred in patients treated with etoricoxib, some of which were fatal.
Caution is advised when treating patients most at risk of developing gastrointestinal complications with NSAIDs: the elderly, patients taking any other NSAIDs or concomitant acetylsalicylic acid, or patients with a history of gastrointestinal disorders such as ulcers and bleeding of the gastrointestinal tract.
When etoricoxib is taken together with acetylsalicylic acid (even at low dose), an additional increased risk of gastrointestinal adverse effects (gastrointestinal ulcer or other gastrointestinal complications) is observed. No significant difference in safety has been demonstrated in long-term clinical studies. gastrointestinal between selective COX-2 inhibitors + acetylsalicylic acid and NSAIDs + acetylsalicylic acid (see section 5.1).
Cardiovascular effects
Clinical studies suggest that the selective COX-2 inhibitor class of drugs may be associated with a risk of thrombotic events (especially MI myocardial infarction and stroke), compared to placebo and some NSAIDs. Since the cardiovascular risks of etoricoxib may increase with dose and duration of exposure, the duration of treatment should be as short as possible and the lowest effective daily dose should be used. The need for treatment and response to therapy should be reassessed periodically, especially in patients with osteoarthritis (see sections 4.2, 4.3, 4.8 and 5.1).
Patients with significant risk factors for cardiovascular events (e.g. hypertension, hyperlipidaemia, diabetes mellitus, smoking habit) should only be treated with etoricoxib after careful consideration (see section 5.1).
Selective COX-2 inhibitors do not replace acetylsalicylic acid in the prophylaxis of thromboembolic cardiovascular disease as they have no antiplatelet effect. Therefore, antiplatelet therapy should not be discontinued (see sections 4.5 and 5.1).
Kidney effects
Renal prostaglandins may play a compensatory role in maintaining renal perfusion. Consequently, in conditions of impaired renal perfusion, administration of etoricoxib may result in a reduction in prostaglandin production and, secondarily, in renal blood flow and thus impair renal function. Patients at the highest risk for this effect are those with pre-existing significant renal impairment, decompensated heart failure or cirrhosis.Renal function monitoring should be considered in such patients.
Fluid retention, edema and hypertension
As with other medicinal products known to inhibit prostaglandin synthesis, fluid retention, edema and hypertension have been observed in patients taking etoricoxib. All Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), including etoricoxib, may be associated with a new onset of congestive heart failure or its recurrence. For information on the dose-related therapeutic response of etoricoxib see section 5.1.
Caution should be exercised in patients with a history of heart failure, left ventricular dysfunction or hypertension and in patients with pre-existing edema for any other reason. If there is clinical evidence of deteriorating condition in these patients, appropriate measures should be taken, including discontinuation of etoricoxib therapy.
Etoricoxib may be associated with more severe and more frequent hypertension than other NSAIDs and selective COX-2 inhibitors, particularly at high doses. Therefore, hypertension should be controlled prior to treatment with etoricoxib (see section 4.3) and special attention should be paid to blood pressure monitoring during treatment with etoricoxib. Blood pressure should be monitored within 2 weeks of initiation of treatment. and then periodically. If blood pressure rises significantly, alternative treatment should be considered.
Hepatic effects
In clinical studies, elevations of alanine aminotransferase (ALT) and / or aspartate aminotransferase (AST) have been reported in approximately 1% of patients treated with 30, 60 and 90 mg per day of etoricoxib for up to one year ( about 3 or more times the upper limit of the norm).
Patient with signs and / or symptoms of liver dysfunction or with abnormal liver function tests should be evaluated. If signs of liver failure are observed or persistent abnormalities (three times higher than normal) in liver function tests are found, treatment with etoricoxib should be discontinued.
Precautions in general
If during the course of treatment patients experience deterioration in the function of any of the organ systems described above, appropriate measures should be taken and discontinuation of etoricoxib therapy should be considered. Elderly patients and those with renal, hepatic or cardiac dysfunction treated with etoricoxib should be kept under adequate medical observation.
Use caution when initiating treatment with etoricoxib in dehydrated patients. It is advisable to rehydrate patients before initiating therapy with etoricoxib.
Serious skin reactions, some of them fatal, including exfoliative dermatitis, Stevens-Johnson syndrome, and toxic epidermal necrolysis, have been reported very rarely in post-marketing experience, in association with the use of NSAIDs and some selective COX-2 inhibitors (see section 4.8). Patients appear to be at higher risk for such reactions during the early phase of therapy, with the onset of symptoms in most cases within the first month of treatment.Serious hypersensitivity reactions (such as anaphylaxis and angioedema) have been reported in patients treated with etoricoxib (see section 4.8). Some selective COX-2 inhibitors have been associated with an increased risk of skin reactions in patients with a history of drug allergy. Treatment with etoricoxib should be discontinued at the appearance of the first signs of skin rash, mucosal lesions or any other signs of hypersensitivity.
Etoricoxib can mask fever and other signs of inflammation.
Caution should be exercised when etoricoxib is administered concomitantly with warfarin or other oral anticoagulants (see section 4.5).
The use of etoricoxib, as with other drugs known to inhibit cyclooxygenase / prostaglandin synthesis, is not recommended in women planning to become pregnant (see sections 4.6, 5.1 and 5.3).
ARCOXIA tablets contain lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption should not take this drug.
04.5 Interactions with other medicinal products and other forms of interaction
Pharmacodynamic interactions
Oral anticoagulants: in subjects stabilized on chronic warfarin therapy, the administration of etoricoxib 120 mg / day was associated with an approximately 13% increase in the International Normalized Ratio (INR) of prothrombin time. Therefore, the INR of prothrombin time of patients receiving oral anticoagulants should be closely monitored, particularly during the very first days, when initiating therapy with etoricoxib or when changing the dose of etoricoxib (see section 4.4).
Diuretics, ACE inhibitors and Angiotensin II-Antagonists (AII-A): NSAIDs may reduce the effect of diuretics and other antihypertensive drugs. In some patients with impaired renal function (eg dehydrated patients or elderly patients with impaired renal function) concomitant administration of an ACE inhibitor or a blood receptor antagonist "angiotensin II and cyclooxygenase inhibiting agents may lead to further deterioration of renal function, including possible acute renal failure, which is usually reversible. These interactions should be considered in patients taking etoricoxib concomitantly with ACE inhibitors or angiotensin II receptor antagonists. The combination should therefore be administered with caution, especially in elderly patients. Patients should be adequately hydrated, with attention to monitoring of renal function at the initiation of concomitant therapy and periodically thereafter.
Acetylsalicylic acid: in a study in healthy individuals, at steady state, etoricoxib 120 mg once daily had no effect on the antiplatelet activity of acetylsalicylic acid (81 mg once daily). Etoricoxib can be used together with acetylsalicylic acid at the doses used for cardiovascular prophylaxis (low-dose acetylsalicylic acid). However, concomitant administration of low dose acetylsalicylic acid with etoricoxib may result in an increased incidence of ulceration of the gastrointestinal tract or other complications compared to etoricoxib alone. Co-administration of etoricoxib with doses of acetylsalicylic acid higher than those described above for cardiovascular prophylaxis or with other NSAIDs is not recommended (see sections 5.1 and 4.4).
Ciclosporin and tacrolimus: although this interaction has not been studied with etoricoxib, concomitant administration of cyclosporine or tacrolimus with any type of NSAID may enhance the nephrotoxic effect of cyclosporine or tacrolimus. Renal function should be monitored when etoricoxib is administered with one of these drugs.
Pharmacokinetic interactions
The effect of etoricoxib on the pharmacokinetics of other drugs
Lithium: NSAIDs reduce renal excretion of lithium and consequently increase plasma lithium concentration. If necessary, carefully monitor blood lithium level and adjust the lithium dose during concomitant drug intake and when treatment with NSAIDs is interrupted.
Methotrexate: two studies evaluated the effects of etoricoxib 60, 90 or 120 mg once daily for seven days in patients receiving rheumatoid arthritis with methotrexate doses of 7.5 to 20 mg once weekly. Etoricoxib at doses of 60 and 90 mg had no effect on plasma methotrexate concentrations or renal clearance. In one study, etoricoxib 120 mg had no effect but in the other study, etoricoxib 120 mg increased the plasma concentrations of methotrexate by 28% and decreased the renal clearance of methotrexate by 13%. Adequate monitoring for toxicity is recommended. from methotrexate when co-administered with methotrexate and etoricoxib.
Oral contraceptives: etoricoxib 60 mg co-administered with an oral contraceptive containing 35 mcg ethinylestradiol (EE) and 0.5 - 1 mg norethindrone for 21 days increased steady-state AUC0-24h of EE by 37%. Etoricoxib 120 mg administered concomitantly with the same oral contraceptive or in separate administrations 12 hours apart, increased the steady-state AUC0-24h of EE by 50 to 60%. This increase in EE concentrations should be taken in consideration when choosing an oral contraceptive to use with etoricoxib. An increase in EE exposure may increase the incidence of adverse events associated with oral contraceptives (eg venous thromboembolic events in women at risk).
Hormone Replacement Therapy (HRT): Administration of etoricoxib 120 mg with conjugated estrogen-based hormone replacement therapy (0.625 mg PREMARIN) for 28 days increased the mean steady-state AUC0-24h of unconjugated estrone (41%), equilin (76%), and 17-β-estradiol (22%). The effect of the recommended chronic doses of etoricoxib (30, 60, and 90 mg) has not been studied. The effects of etoricoxib 120 mg on exposure (AUC0-24h) to the above estrogenic components of PREMARIN were less than half the effects. observed with administration of PREMARIN alone and the dose was increased from 0.625 to 1.25 mg. The clinical significance of these increases is unknown, and higher doses of PREMARIN have not been studied in combination with etoricoxib. Such increases in estrogen concentration should be considered when selecting postmenopausal hormone replacement therapy for use with etoricoxib as increased exposure to estrogen may increase the risk of adverse events associated with HRT.
Prednisone / prednisolone: in drug interaction studies, etoricoxib had no clinically relevant effect on the pharmacokinetics of prednisone / prednisolone.
Digoxin: etoricoxib 120 mg once daily for 10 days to healthy volunteers did not alter plasma steady-state AUC0-24h or "renal elimination of digoxin. C" was an increase in digoxin Cmax (approximately 33%). This increase was generally not relevant for most patients. However, patients at high risk for digoxin toxicity should be monitored for co-administration of etoricoxib and digoxin.
Effects of etoricoxib on drugs metabolised by sulfotransferases
Etoricoxib is an inhibitor of human sulfotransferase activity, particularly SULT1E1, and has been shown to increase the serum concentrations of ethinylestradiol. Although knowledge on the effects of several sulfotransferases is currently limited and the clinical consequences for many drugs are still under investigation, it may be prudent to exercise caution when coadministration of etoricoxib with other drugs metabolised primarily by human sulfotransferases (e.g. salbutamol and minoxidil per os).
Effects of etoricoxib on drugs metabolised by isoenzymes of the CYP system
Based on studies in vitro, etoricoxib is not expected to inhibit cytochromes P450 (CYP) 1A2, 2C9, 2C19, 2D6, 2E1 or 3A4. In a study in healthy subjects, daily administration of 120 mg etoricoxib did not alter CYP3A4 liver activity as measured by the erythromycin breath test.
Effect of other drugs on etoricoxib pharmacokinetics
The major metabolic pathway of etoricoxib depends on CYP enzymes. CYP3A4 appears to contribute to the metabolism of etoricoxib in vivo. Education in vitro indicate that CYP2D6, CYP2C9, CYP1A2 and CYP2C19 can also catalyze the major metabolic pathway, but their quantitative roles have not yet been studied in vivo.
Ketoconazole: ketoconazole, a potent CYP3A4 inhibitor, once daily of 400 mg for 11 days to healthy volunteers, had no clinically relevant effect on the single dose pharmacokinetics of 60 mg etoricoxib (43% increase in AUC).
Voriconazole and Miconazole: concomitant administration of oral voriconazole or topical miconazole oral gel, strong inhibitors of CYP3A4, with etoricoxib caused a slight increase in etoricoxib exposure, but is not considered to be clinically significant based on published data.
Rifampicin: Concomitant administration of etoricoxib with rifampicin, a potent inducer of CYP enzymes, resulted in a 65% decrease in plasma concentrations of etoricoxib. This interaction may result in relapse of symptoms when etoricoxib is co-administered with rifampicin. While this may suggest a dose increase, doses of etoricoxib higher than those anticipated for each indication have not been studied in combination with rifampicin and are therefore not recommended (see section 4.2).
Antacids: antacids do not affect the pharmacokinetics of etoricoxib to a clinically significant extent.
04.6 Pregnancy and lactation
Pregnancy
There are no clinical data on exposure to etoricoxib in pregnant women. Studies in animals have shown reproductive toxicity (see section 5.3). The potential risk in pregnant women is unknown. Etoricoxib, like other medicinal products that inhibit prostaglandin synthesis, it can cause uterine inertia and premature closure of the arterial duct during the last trimester. Etoricoxib is contraindicated in pregnancy (see section 4.3). If pregnancy occurs during treatment, etoricoxib therapy should be discontinued.
Feeding time
It is not known whether etoricoxib is excreted in human milk. Etoricoxib is excreted in rat milk. Women taking etoricoxib must not breastfeed (see sections 4.3 and 5.3).
Fertility
The use of etoricoxib, like that of other pharmacological substances known to inhibit COX-2, is not recommended in women planning to become pregnant.
04.7 Effects on ability to drive and use machines
Patients who experience dizziness, vertigo or somnolence when taking etoricoxib should refrain from driving or operating machinery.
04.8 Undesirable effects
Summary of the safety profile
In clinical studies, etoricoxib was evaluated for safety in 7,152 individuals, including 4,614 patients with OA, RA, chronic low back pain or ankylosing spondylitis (approximately 600 patients with OA or RA were treated for one year or more).
In clinical studies, the undesirable effect profile was similar in patients with OA or RA treated with etoricoxib for one year or longer.
In a clinical study in acute gouty arthritis, patients were treated with etoricoxib 120 mg once daily for 8 days. The adverse experience profile in this study was generally similar to the combined outcome reported in the OA, RA and low back pain studies. chronic.
In an outcome-based cardiovascular safety study program, where pooled data from three active comparator controlled trials were evaluated, 17,412 patients with OA or RA were treated with etoricoxib (60 mg or 90 mg ) for an average duration of approximately 18 months. Safety data and details from this study are presented in section 5.1.
In clinical trials of acute postoperative dental pain following surgery which included 614 patients treated with etoricoxib (90 mg or 120 mg), the adverse experience profile in these studies was generally similar to that reported in the combined OA, RA studies. , and chronic low back pain.
Table of adverse reactions
The following undesirable effects were reported in clinical trials, with a "higher incidence than placebo in patients with OA, RA, chronic low back pain or ankylosing spondylitis treated with etoricoxib 30 mg, 60 mg or 90 mg up to the recommended dose for up to at 12 weeks; in MEDAL program studies up to 3½ years, in short-term acute pain studies up to 7 days; or in post-marketing experience (see Table 1):
Table 1:
The following serious undesirable effects have been reported in association with the use of NSAIDs and cannot be excluded with etoricoxib: nephrotoxicity including interstitial nephritis, nephrotic syndrome.
04.9 Overdose
In clinical studies, single doses of etoricoxib up to 500 mg and multiple doses up to 150 mg / day for 21 days did not result in significant toxicity. There have been reports of acute overdose with etoricoxib, although no adverse experiences were reported in the majority of cases. The most frequently observed adverse experiences were consistent with the safety profile of etoricoxib (e.g., gastrointestinal events, cardiorenal events).
In the event of an overdose, it is reasonable to take common supportive measures, such as removing unabsorbed material from the GI tract, clinically monitoring the patient and instituting supportive care if necessary.
Etoricoxib is not dialysable by hemodialysis; it is not known whether etoricoxib is dialysable by peritoneal dialysis.
05.0 PHARMACOLOGICAL PROPERTIES
05.1 Pharmacodynamic properties
Pharmacotherapeutic group: anti-inflammatory and antirheumatic drugs, non-steroids, coxibs.
ATC code: M01 AH05.
Mechanism of action
Etoricoxib is a selective inhibitor of cyclooxygenase 2 (COX-2) within the clinical dose range, for oral administration.
In all clinical pharmacology studies, ARCOXIA resulted in dose-dependent inhibition of COX-2 without inhibition of COX-1 at doses up to 150 mg / day. Etoricoxib did not inhibit gastric prostaglandin synthesis and had no effect on platelet function.
Cyclooxygenase is responsible for the production of prostaglandins. Two isoforms have been identified, COX-1 and COX-2. COX-2 is the "isoform" of the enzyme that has been shown to be induced by proinflammatory stimuli and is believed to be primarily responsible for the synthesis of prostanoid mediators of pain, inflammation and fever. COX-2 is also involved in ovulation, in the implantation of the embryo and in the closure of the arterial duct, in the regulation of renal function and in some functions of the central nervous system (induction of fever, pain perception and cognitive function). It can also play a role in ulcer healing. COX-2 has been identified in the tissues surrounding gastric ulcers in humans but its relevance in healing ulcers has not been established.
Clinical efficacy and safety
Effectiveness
In patients with osteoarthritis (OA), etoricoxib 60 mg once daily resulted in significant improvements in pain and patient assessment of disease status. These positive effects were seen as early as the second day of therapy and lasted for up to 52 weeks. Studies with etoricoxib 30 mg once daily demonstrated superior efficacy to placebo over the 12-week treatment period (using similar evaluations to the above studies). In a dose ranging study, etoricoxib 60 mg demonstrated a Significantly greater improvement over 30 mg in all 3 primary endpoints over the 6-week treatment period. The 30 mg dose has not been studied in osteoarthritis of the hands.
In patients with rheumatoid arthritis (RA), etoricoxib 90 mg once daily resulted in significant improvements in pain, inflammation and mobility. These positive effects were maintained throughout the 12-week treatment periods.
In patients with acute gouty arthritis attacks, etoricoxib 120 mg once daily for an eight-day treatment period provided moderate to considerable relief of joint pain and inflammation compared to indomethacin 50 mg three times daily. pain relief was seen as early as four hours after starting treatment.
In patients with ankylosing spondylitis, etoricoxib 90 mg once daily provided significant improvements in spine pain, inflammation, stiffness and function. The clinical benefit of etoricoxib therapy was seen as early as the second day of therapy and was maintained throughout the 52-week treatment period.
In a clinical study evaluating postoperative dental pain, etoricoxib 90 mg was administered once daily for up to three days. In the subgroup of patients with moderate pain at baseline, etoricoxib 90 mg exhibited an analgesic effect similar to that of ibuprofen 600 mg (16.11 vs. 16.39; P = 0.722), and superior to that of paracetamol / codeine 600 mg / 60 mg (11.00; P
Safety
MEDAL Program (Multinational Etoricoxib and Diclofenac Arthritis Long-term)
The MEDAL Program was a prospective study program on outcome cardiovascular (CV) safety from pooled data from three randomized, double-blind, active comparator controlled clinical trials, the MEDAL, EDGE II, and EDGE trials.
The MEDAL study was a study on outcome CV conducted on 17,804 patients with OA and 5,700 patients with RA treated with etoricoxib 60 (OA) or 90 mg (OA and RA) or diclofenac 150 mg / day for a mean period of 20.3 months (maximum of 42.3 months , median 21.3 months). Only serious adverse events and discontinuations due to any adverse event were recorded in this study.
The EDGE and EDGE II studies compared the gastrointestinal tolerability of etoricoxib vs diclofenac. The EDGE study included 7,111 patients with OA treated with a dose of etoricoxib 90 mg / day (1.5 times the recommended dose for OA) or diclofenac 150 mg / day for a mean period of 9.1 months (maximum 16 , 6 months, median 11.4 months). The EDGE II study included 4,086 RA patients treated with etoricoxib 90 mg / day or diclofenac 150 mg / day for a mean of 19.2 months (maximum 33.1 months, median 24 months).
In the MEDAL pooled data program, 34,701 patients with OA or RA were treated for a mean duration of 17.9 months (maximum 42.3 months, median 16.3 months), with approximately 12,800 patients being treated for more than 24 months. Patients enrolled in the Program had a large range of cardiovascular and gastrointestinal risk factors at baseline. Patients with a recent history of myocardial infarction, coronary artery bypass graft or PCI within 6 months prior to enrollment were excluded. The use of gastroprotective agents and low-dose aspirin were permitted in the studies.
Global security:
There was no significant difference between the cardiovascular thrombotic event rates of etoricoxib and those of diclofenac. Cardiorenal adverse events were observed more frequently with etoricoxib than with diclofenac, and this effect was dose-dependent (see specific results below). Gastrointestinal and hepatic adverse events were observed significantly more frequently with diclofenac than with etoricoxib. The incidence of adverse experiences in EDGE and EDGE II and of adverse experiences considered serious or likely to lead to discontinuation in the MEDAL study was higher with etoricoxib than with diclofenac.
Cardiovascular Safety Results:
The incidence of serious confirmed thrombotic cardiovascular adverse events (cardiac, cerebrovascular and peripheral vascular events) was comparable between etoricoxib and diclofenac, and the data are summarized in the table below. There were no statistically significant differences in the incidence of thrombotic events with etoricoxib and diclofenac in all subgroups analyzed including all categories of patients with baseline cardiovascular risk. The relative risks for confirmed serious thrombotic cardiovascular adverse events considered separately with etoricoxib 60 mg or 90 mg versus diclofenac 150 mg were similar.
CV mortality and overall mortality were similar between the etoricoxib and diclofenac treatment groups.
Cardiorenal events:
Approximately 50% of patients enrolled in the MEDAL study had a history of hypertension at baseline. In the study, the incidence of discontinuations due to hypertension-related adverse events was statistically significantly higher for etoricoxib than for diclofenac. The incidence of adverse events for congestive heart failure (interruptions and serious events) occurred at similar rates with etoricoxib 60 mg compared to diclofenac 150 mg, but was higher for etoricoxib 90 mg than diclofenac 150 mg (statistically significant for etoricoxib 90 mg vs. diclofenac 150 mg in the MEDAL OA cohort). The incidence of confirmed adverse events for congestive heart failure (serious events leading to hospitalization or an emergency department visit) was significantly higher. not significant with etoricoxib compared to diclofenac 150 mg, and this effect was dose-dependent. The incidence of discontinuations due to edema-related adverse events was higher for etoricoxib than for diclofenac 150 mg, and this effect was dose-dependent (statistically significant for etoricoxib 90 mg, but not for etoricoxib 60 mg).
The cardiorenal results for EDGE and EDGE II were in line with those described for the MEDAL study.
In individual studies of the MEDAL program, the absolute incidence of discontinuations in all treatment groups for etoricoxib (60 mg or 90 mg) was up to 2.6% for hypertension, up to 1.9% for edema, and up to 1.1% for congestive heart failure, with higher discontinuation rates observed with etoricoxib 90 mg compared to etoricoxib 60 mg.
Gastrointestinal tolerability results of the MEDAL program:
Within each of the three studies part of the MEDAL program, a significantly lower discontinuation rate was observed for etoricoxib than for diclofenac for all GI adverse clinical events (eg, dyspepsia, abdominal pain, ulcer). discontinuation due to GI adverse clinical events per 100 patient-years over the entire study period were as follows: 3.23 for etoricoxib and 4.96 for diclofenac in the MEDAL study; 9.12 with etoricoxib and 12.28 with diclofenac in the EDGE study; and 3.71 with etoricoxib and 4.81 with diclofenac in the EDGE II study.
Gastrointestinal safety results of the MEDAL program:
Upper GI events were defined as perforations, ulcers and bleeding. The subset of all upper GI events considered complicated included perforations, obstructions, and complicated bleeding; the subset of upper GI events considered uncomplicated included uncomplicated bleeding and uncomplicated ulcers. A significantly lower overall GI event rate was observed with etoricoxib than with diclofenac. There was no significant difference between etoricoxib and diclofenac with respect to the complicated event rate. For the subgroup of upper GI bleeding events (combined complicated and uncomplicated data), there was no significant difference between etoricoxib and diclofenac. In patients on concomitant low-dose aspirin therapy (approximately 33% of patients ) there was no significant benefit with etoricoxib over diclofenac in the upper GI tract.
The per 100 patient-years rates of confirmed complicated and uncomplicated upper GI events (perforations, ulcers and bleeding (PUBs)) were 0.67 (95% CI 0.57, 0.77) with etoricoxib and 0.97 (95% CI 0.85, 1.10) with diclofenac, resulting in a relative risk of 0.69 (95% CI 0.57, 0.83).
The rate of confirmed upper GI events in elderly patients was evaluated and the largest reduction was seen in patients ≥75 years of age, 1.35 [95% CI 0.94, 1.87] vs. 2.78 [95% CI 2.14, 3.56] events per 100 patient-years for etoricoxib and diclofenac, respectively.
The rates of confirmed clinical events affecting the lower GI tract (perforation, obstruction or haemorrhage of the small or large intestine (POB)), were not significantly different between etoricoxib and diclofenac.
MEDAL program liver safety results:
Etoricoxib was associated with a significantly lower rate of discontinuation due to hepatic adverse experiences than diclofenac. In the combined data from the MEDAL program, 0.3% of patients receiving etoricoxib and 2.7% of patients receiving diclofenac discontinued due to hepatic adverse events.
The rate per 100 patient-years was 0.22 for etoricoxib and 1.84 for diclofenac (p-value was
Additional safety data relating to cardiovascular thrombotic events
In clinical trials excluding the MEDAL program studies, approximately 3,100 patients were treated with etoricoxib ≥ 60 mg / day for 12 weeks or longer. There were no appreciable differences in the rate of serious confirmed thrombotic cardiovascular events between patients treated with etoricoxib ≥ 60 mg, placebo, or NSAIDs excluding naproxen. However, the incidence of these events was higher in patients treated with etoricoxib than in those treated with naproxen 500 mg twice daily. The difference in antiplatelet activity between some COX-1 inhibitor NSAIDs and COX-2 selective inhibitors may affect clinical significance in patients at risk for thromboembolic events COX-2 inhibitors reduce systemic (and therefore possibly endothelial) prostacyclin formation without affecting platelet thromboxane The clinical relevance of these findings has not been established.
Additional gastrointestinal safety data
In two 12-week double-blind endoscopy studies, the cumulative incidence of gastrointestinal ulcers was significantly lower in patients treated with etoricoxib 120 mg once daily compared to patients treated with naproxen 500 mg twice daily or ibuprofen 800 mg three. times a day Etoricoxib had a higher incidence of gastrointestinal ulcers than placebo.
Renal function study in the elderly
The effects of 15 days of treatment with etoricoxib (90 mg), celecoxib (200 mg bid), naproxen (500 mg bid) and placebo on urinary sodium excretion, blood pressure, and other renal function parameters in subjects aged 60 and 85 years on a dietary regimen of 200 mEq / day of sodium, were evaluated in a randomized, double-blind, placebo-controlled parallel group study. Etoricoxib, celecoxib, and naproxen had similar effects on urinary sodium excretion over 2 weeks of treatment. All active comparators showed an increase in systolic blood pressure values compared to placebo; however, etoricoxib was associated with an increase. statistically significant at day 14 compared to celecoxib and naproxen (mean change from baseline for systolic blood pressure: etoricoxib 7.7 mmHg, celecoxib 2.4 mmHg, naproxen 3.6 mmHg).
05.2 Pharmacokinetic properties
Absorption
Orally administered etoricoxib is well absorbed. The mean bioavailability after oral administration is approximately 100%. With once daily administration of 120 mg, the peak plasma concentration (geometric mean Cmax = 3.6 μg / ml) steady state was observed approximately 1 hour (Tmax) after dosing in fasted adults. The geometric mean of the area under the curve (AUC0-24h) was 37.8 mcg • h / ml. The pharmacokinetics of etoricoxib are linear across the clinical dose spectrum.
Food intake (a high-fat meal) had no effect on the extent of absorption from a 120 mg dose of etoricoxib. The rate of absorption was altered, with a 36% decrease in Cmax and a two-hour increase in Tmax. These data are not considered clinically significant. In clinical studies, etoricoxib was administered without regard to food.
Distribution
Etoricoxib is approximately 92% bound to human plasma proteins at concentrations ranging from 0.05 to 5 mcg / ml. In humans, the steady-state volume of distribution (Vdss) was approximately 120 l.
Etoricoxib crosses the placenta in the rat and rabbit, and the blood brain barrier in the rat.
Metabolism
Etoricoxib is extensively metabolised in urine as parent drug. The major metabolic pathway for the formation of the 6-hydroxymethyl derivative is catalysed by CYP enzymes.CYP3A4 appears to contribute to the metabolism of etoricoxib in vivo. Education in vitro indicate that CYP2D6, CYP2C9, CYP1A2 and CYP2C19 can also catalyze the major metabolic pathway, but their role quantitatively has not been studied in vivo.
Five metabolites have been identified in humans. The major metabolite is the 6 "-carboxylic acid derivative of etoricoxib formed by the" further oxidation of the 6 "-hydroxymethyl derivative. These major metabolites either showed no measurable activity or showed only weak activity. as COX-2 inhibitors None of these metabolites inhibit COX-1.
Elimination
Following administration of a single 25 mg intravenous dose of radiolabelled etoricoxib to healthy subjects, 70% of the radioactivity was detected in the urine and 20% in the faeces, mostly in the form of metabolites. Less than 2% was found as unchanged drug.
Elimination of etoricoxib occurs almost exclusively via metabolism followed by renal excretion. Steady-state concentrations of etoricoxib are achieved within seven days with once daily administration of 120 mg, with an accumulation rate of approximately 2, corresponding to an accumulation half-life of approximately 22 hours. Plasma clearance is estimated to be approximately 50 ml / min following an intravenous dose of 25 mg.
Characteristics of patients
Senior citizens: in the elderly (65 years of age and older) the pharmacokinetics are similar to that of the young.
Sex: the pharmacokinetics of etoricoxib are similar in men and women.
Liver failure: in patients with mild hepatic dysfunction (Child-Pugh score 5-6) once daily administration of 60 mg etoricoxib resulted in a mean AUC approximately 16% higher than that in healthy subjects given the same dose. In patients with moderate hepatic dysfunction (Child-Pugh score 7-9) administered 60 mg etoricoxib every other day, Mean AUC was similar to healthy subjects given etoricoxib 60 mg once daily; etoricoxib 30 mg once daily has not been studied in this population. There are no clinical or pharmacokinetic data in patients with severe dysfunction. liver (Child-Pugh score ≥10), (see sections 4.2 and 4.3).
Kidney failure: the pharmacokinetics of a single 120 mg dose of etoricoxib in patients with moderate to severe renal impairment and in hemodialysis patients with end stage renal disease were not significantly different from that of healthy subjects. Hemodialysis contributed negligibly to elimination (dialysis clearance approximately 50 ml / min) (see sections 4.3 and 4.4).
Pediatric patients: the pharmacokinetics of etoricoxib in pediatric patients (
In a pharmacokinetic study (n = 16) conducted in adolescents (ages 12-17), pharmacokinetics in adolescents weighing 40-60 kg treated with etoricoxib 60 mg once daily and adolescents> 60 kg treated with etoricoxib 90 mg once daily was similar to that in adults treated with etoricoxib 90 mg once daily. Safety and efficacy of etoricoxib in pediatric patients have not been established (see section 4.2).
05.3 Preclinical safety data
In preclinical studies, etoricoxib was shown not to be genotoxic. Etoricoxib was not carcinogenic in mice. Rats treated daily for approximately two years at doses> 2 times the human daily dose [90 mg] based on systemic exposure developed hepatocellular adenomas and follicular adenomas of the thyroid gland. These types of tumors observed in rats are considered to be a species-specific consequence of the induction of hepatic CYP enzymes in the rat. Etoricoxib has not been shown to induce hepatic CYP3A enzyme induction in humans.
In the rat, the gastrointestinal toxicity of etoricoxib increased with dose and time of exposure. In a 14-week rat toxicity study, etoricoxib caused gastrointestinal ulcers at doses above the human therapeutic dose. In the 53- and 106-week toxicity study, gastrointestinal ulcers were also observed at exposures comparable to those observed in humans at therapeutic doses. At high exposures, renal and gastrointestinal alterations were observed in dogs.
Etoricoxib was not teratogenic in reproductive toxicity studies conducted in rats at 15 mg / kg / day (exposure approximately 1.5 times the human daily dose [90 mg] based on systemic exposure). In rabbits, a dose-related increase in cardiovascular malformations was observed at exposure levels below the clinical exposure achievable in humans at the daily dose (90 mg). However, no treatment-related fetal skeletal or external malformations were observed. In rats and rabbits, there was a dose-related increase in post-implantation loss at exposures greater than or equal to 1.5 times the human exposure (see sections 4.3 and 4.6).
Etoricoxib is excreted in the milk of lactating rats at concentrations approximately twice that of plasma. There was weight loss in offspring exposed to milk from lactating animals treated with etoricoxib.
06.0 PHARMACEUTICAL INFORMATION
06.1 Excipients
Inside of the tablets:
Anhydrous dibasic calcium phosphate
Croscarmellose sodium
Magnesium stearate
Microcrystalline cellulose
Coating of tablets:
Carnauba wax
Lactose monohydrate
Hypromellose
Titanium dioxide (E171)
Triacetin
The 30, 60 and 120 mg tablets also contain indigo carmine lake (E132) and yellow iron oxide (E172).
06.2 Incompatibility
Not relevant.
06.3 Period of validity
3 years.
06.4 Special precautions for storage
Bottles: Keep container tightly closed to protect from moisture.
Blisters: Store in the original package to protect from moisture.
06.5 Nature of the immediate packaging and contents of the package
30 mg
Aluminum / aluminum blisters in packs of 2, 7, 14, 20, 28, 49 tablets or multi-packs of 98 (2 packs of 49) tablets.
60, 90 and 120 mg
Aluminum / aluminum blisters in packs of 2, 5, 7, 10, 14, 20, 28, 30, 50, 84, 100 tablets or multi-packs of 98 (2 packs of 49) tablets.
Aluminum / aluminum blisters (single dose) in packs of 5, 50 and 100 tablets.
White, round, HDPE bottles with white polypropylene closure containing 30 tablets with two 1 gram desiccant containers and 90 tablets with one 1 gram desiccant container.
Not all pack sizes may be marketed.
06.6 Instructions for use and handling
No special instructions.
07.0 MARKETING AUTHORIZATION HOLDER
MSD Italia S.r.l.
Via Vitorchiano, 151 - 00189 Rome
08.0 MARKETING AUTHORIZATION NUMBER
"30 mg film-coated tablets" 7 tablets in blister Al / Al AIC n.035820442 / M
"30 mg film-coated tablets" 28 tablets in Al / Al blister AIC n.035820430 / M
"60 mg film-coated tablets" 2 tablets in blister Al / Al AIC n.035820012 / M
"60 mg film-coated tablets" 5 tablets in blister Al / Al AIC n.035820024 / M
"60 mg film-coated tablets" 7 tablets in blister Al / Al AIC n.035820036 / M
"60 mg film-coated tablets" 10 tablets in blister Al / Al AIC n.035820048 / M
"60 mg film-coated tablets" 14 tablets in blister Al / Al AIC n.035820051 / M
"60 mg film-coated tablets" 20 tablets in blister Al / Al AIC n.035820063 / M
"60 mg film-coated tablets" 28 tablets in blister Al / Al AIC n. 035820075 / M
"60 mg film-coated tablets" 30 tablets in blister Al / Al AIC n. 035820087 / M
"60 mg film-coated tablets" 50 tablets in blister Al / Al AIC n. 035820099 / M
"60 mg film-coated tablets" 98 (2x49) tablets in blister Al / Al AIC n. 035820101 / M
"60 mg film-coated tablets" 100 tablets in blister Al / Al AIC n. 035820113 / M
"60 mg film-coated tablets" 50x1 tablets in blister Al / Al AIC n. 035820125 / M
"60 mg film-coated tablets" 100x1 tablets in blister Al / Al AIC n. 035820137 / M
"60 mg film-coated tablets" 30 tablets in HDPE bottle AIC n. 035820149 / M
"90 mg film-coated tablets" 2 tablets in blister Al / Al AIC n. 035820152 / M
"90 mg film-coated tablets" 5 tablets in blister Al / Al AIC n. 035820164 / M
"90 mg film-coated tablets" 7 tablets in blister Al / Al AIC n. 035820176 / M
"90 mg film-coated tablets" 10 tablets in blister Al / Al AIC n. 035820188 / M
"90 mg film-coated tablets" 14 tablets in blister Al / Al AIC n. 035820190 / M
"90 mg film-coated tablets" 20 tablets in blister Al / Al AIC n. 035820202 / M
"90 mg film-coated tablets" 28 tablets in blister Al / Al AIC n. 035820214 / M
"90 mg film-coated tablets" 30 tablets in blister Al / Al AIC n. 035820226 / M
"90 mg film-coated tablets" 50 tablets in blister Al / Al AIC n. 035820238 / M
"90 mg film-coated tablets" 98 (2x49) tablets in blister Al / Al AIC n. 035820240 / M
"90 mg film-coated tablets" 100 tablets in blister Al / Al AIC n. 035820253 / M
"90 mg film-coated tablets" 50x1 tablets in blister Al / Al AIC n. 035820265 / M
"90 mg film-coated tablets" 100x1 tablets in blister Al / Al AIC n. 035820277 / M
"90 mg film-coated tablets" 30 tablets in HDPE bottle AIC n. 035820289 / M
"120 mg film-coated tablets" 2 tablets in blister Al / Al AIC n. 035820291 / M
"120 mg film-coated tablets" 5 tablets in blister Al / Al AIC n. 035820303 / M
"120 mg film-coated tablets" 7 tablets in blister Al / Al AIC n. 035820315 / M
"120 mg film-coated tablets" 10 tablets in blister Al / Al AIC n. 035820327 / M
"120 mg film-coated tablets" 14 tablets in blister Al / Al AIC n. 035820339 / M
"120 mg film-coated tablets" 20 tablets in blister Al / Al AIC n. 035820341 / M
"120 mg film-coated tablets" 28 tablets in blister Al / Al AIC n. 035820354 / M
"120 mg film-coated tablets" 30 tablets in blister Al / Al AIC n. 035820366 / M
"120 mg film-coated tablets" 50 tablets in blister Al / Al AIC n. 035820378 / M
"120 mg film-coated tablets" 98 (2x49) tablets in blister Al / Al AIC n. 035820380 / M
"120 mg film-coated tablets" 100 tablets in blister Al / Al AIC n. 035820392 / M
"120 mg film-coated tablets" 50x1 tablets in blister Al / Al AIC n. 035820404 / M
"120 mg film-coated tablets" 100x1 tablets in blister Al / Al AIC n. 035820416 / M
"120 mg film-coated tablets" 30 tablets in HDPE bottle AIC n. 035820428 / M
09.0 DATE OF FIRST AUTHORIZATION OR RENEWAL OF THE AUTHORIZATION
February 2004 / February 2012
10.0 DATE OF REVISION OF THE TEXT
May 2013