The spermiogram is a laboratory test aimed at the study of seminal fluid, still today considered a basic tool in the evaluation of male fertility. The answers provided by the spermiogram on reproductive capacity are however not definitive, since it is an in vitro study that may not reflect the behavior of the seminal fluid in the female reproductive system. Furthermore, the study of the spermiogram refers to a single ejaculation and it may happen, for example, that in that particular episode the number of spermatozoa is only occasionally lower than the limits considered normal, or that the fertilizing capacity is in any case maintained. Despite these limitations, the spermiogram remains an important first level test for the classification of male infertility.

The fundamental contribution of the patient to the success of the spermiogram
In order for the results of the spermiogram to be reliable, it is essential that the patient respects some basic rules. In particular, it is required:
- complete abstinence from sexual activity not less than three days and not more than five days.
- Ejaculation obtained exclusively by masturbation (avoiding, unless otherwise instructed, the use of a condom or the technique of interrupted coitus).
- Before masturbation, proceed with adequate hand and penis hygiene.
- Collect the entire release of seminal fluid in the sterile jar; after ejaculation, squeeze the penis to release all the seminal fluid from the urethra.
- Use suitable and sterile containers (generally wide mouth urine collectors are used, with a label with the name of the patient).
- Carefully close the container to prevent accidental loss of the sample during transport and delivery.
- After ejaculation, have the sample prevented by the analysis laboratory within 30/60 minutes, saving him from thermal shocks (less than 20 ° C and more than 40 ° C). For these reasons, when possible, the collection of the sample should be carried out directly at the lab.
- Report any treatments and illnesses (particularly with fever) that have occurred in the past three months to the healthcare professional. Also report any loss of the sample during collection or transport, and any other violation of the rules listed above.
What does the exam consist of?
During the spermiogram three fundamental parameters of the seminal fluid are studied: concentration (number), motility (ability to move) and morphology (shape) of the spermatozoa. These three characteristics influence the fertilizing capacity of the same, that is the ability to go up the cervix and the uterus to the site of the egg cell, undergo capacitation (a series of transformations that increases the fertilizing capacity), penetrate the corona radiata, sacrifice oneself in order to undermine the resistance of the zona pellucida and allow a single sperm to open a passage towards the nucleus, where it will combine its genetic heritage with that of the oocyte.
The results of the spermiogram
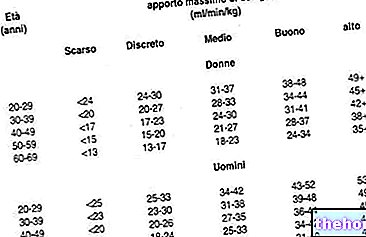
The World Health Organization (WHO) considers an ejaculate to be normal with:
Other reference parameters: fructose:> 13 µmol / ejaculate; seminal pH: 7.2-8.0; white blood cells: less than 1 million / ml.
Note: the normal ranges may vary from laboratory to laboratory, also in relation to the bibliographic sources consulted.
Possible results of the spermiogram:
- Normozoospermia: normal ejaculate, according to reference values.
- Astenozoospermia: alteration of the motility of spermatozoa.
- Oligozoospermia (or simply oligospermia): reduced number of spermatozoa.
- Cryptospermia: severe sperm deficiency (absence of sperm in the ejaculate but presence of sperm in the centrifuged).
- Azoospermia: absence of spermatozoa in seminal fluid.
- Teratozoospermia: alteration of the morphology of spermatozoa.
- Hypospermia or oligoposia or hypoposia: reduction of the ejaculate volume.
- Hyperposia: increased ejaculate volume.
Oligoastenoteratozoospermia: alteration of all variables.
The results of the spermiogram, considering the premise made at the beginning of the article, must be confirmed in two subsequent examinations, collected in an interval between one week and three months. A third sample must be collected at least one quarter after the first spermiogram, in order to have a totally new sperm population available for analysis (since the maturation time of the male germ cells is about 75 days, followed by another 10- 15 days of epididymal maturation). This last consideration also makes it necessary - in order to verify the results of any therapies undertaken - to wait at least three months from their beginning before repeating the spermiogram.













.jpg)











