Generality
The term megacolon identifies an "abnormal distension that affects the colon in its entirety or a specific portion of it. The causes can be congenital, therefore present from birth (Hirschsprung's disease), or acquired (megacolon is secondary to other diseases, such as colitis colitis, infectious colitis, intestinal obstructions or sub-obstructions often resulting from stubborn constipation). Other times, colic excessive dilation arises without any obvious cause (idiopathic megacolon) or is favored by drugs that reduce intestinal peristalsis - such as antidiarrheals, anticholinergics and narcotics - or from prolonged antibiotic therapies (this is the specific case of Clostridium difficile pseudomembranous colitis).
The severity of the megacolon depends on its origins; the condition is extremely dangerous in acute onset toxic forms, while it appears mild and easier to resolve in case of partial obstruction resulting from chronic constipation.

Symptoms
When we talk about megacolon, we often only remember the symptoms associated with acute and toxic forms, including abdominal pain and distension, absence or scarcity of intestinal peristalsis and symptoms of systemic toxicity (such as mental confusion). In fact, given the wide spread of constipation, a modest colic distension is appreciable in many people, even in children. difficult and painful defecation, tends to cause anal hyperdistension and consequent cracking of the mucosa (fissures), accompanied by pain and traces of bright red blood in the toilet paper. Especially in children, pain can lead to a vicious circle in which defecation is interpreted as a painful act, for which we tend to ignore and postpone the stimuli, fueling constipation and favoring the appearance of chronic megacolon.
Hirschsprung's disease
Hirschsprung's disease has an "estimated incidence of one case in every 5,000 live births, and affects males four times as often as females. Although its origins are still to be clarified, the disease seems to recognize an autosomal dominant component ( given the tendency to occur more frequently in some families).
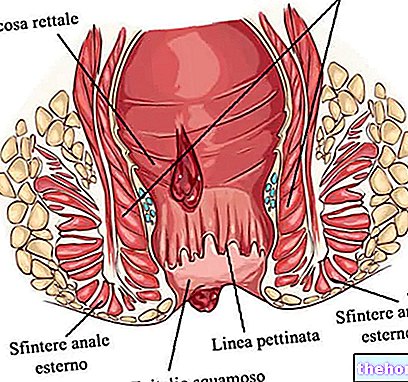
It is characterized by developmental and maturation anomalies of the Enteric Nervous System, also known as "second brain" or "gut mini brain". Due to the lack of ganglia of the rectum or rectus sigma, there is a reduction in peristalsis of the intestine. The affected tract is unable to relax and to cause peristaltic movements, with a slowing of the progression of the enteric content and consequent distension.
The treatment of choice is surgical resection of the aganglionic intestinal segment.
Secondary megacolon
Toxic and non-toxic forms are distinguished.
- ACUTE TOXIC MEGACOLON: it is a typical consequence of inflammatory bowel diseases (ulcerative colitis and more rarely Crohn's disease), toxic colitis or infectious colitis; the term "toxic" underlines the presence of symptoms of systemic toxicity (such as mental confusion) attributable to alterations in electrolyte homeostasis and acid-base balance.
- NON-TOXIC MEGACOLON: often resulting from chronic mechanical obstruction or subocclusion, common in case of stubborn constipation (in this case colic dilation is observed upstream of the obstruction).
Sometimes, although the signs, symptoms and radiological findings suggest it, it is not possible to identify the obstruction; this is the case of Ogilvie's syndrome, typical of hospitalized patients and associated with a "wide range of metabolic, pharmacological or post -operatives that suppress colon motility.
Treatment of these forms of megacolon aims to reduce the distension of the colon to prevent perforation. This result is obtained by aspiration through a nasogastric tube and rectal tube. Mouth feeding is suspended to avoid the introduction of air and food; it is then replaced by enteral nutrition, with particular attention to restoring the electrolyte balance to prevent shock and dehydration.
All diagnostic and therapeutic procedures must be carried out with extreme care after evaluating the risk of intestinal perforation; laxatives and evacuative enemas, for example, can be useful to prevent the appearance of megacolon from fecalomas, but are contraindicated in the presence of toxic megacolon or severe acute distension.
Among the drugs useful in the presence of megacolon we remember:
- corticosteroids: can be useful for suppressing the inflammatory reaction when toxic megacolon is caused by the exacerbation of an inflammatory bowel disease.
- Broad-spectrum antibiotics: given intravenously, they can be used to prevent sepsis or to treat toxic megacolon dependent on Clostridium difficile infections
- Drugs that stimulate peristalsis are sometimes useful (eg neostigmine, used in case of Ogilvie's syndrome);
- Withdrawal of drugs that can reduce colon motility (e.g. narcotics, antidiarrheals, anticholinergics, calcium channel antagonists)
In the presence of a particularly important distension subject to the risk of perforation, or in the event of failure of the therapies described above, to resolve megacolon, surgical removal of a more or less extensive part of the colon (colectomy) is required.