Edited by Dr. Andrea Gizdulich
The most recent knowledge of neuromuscular pathophysiology has shown that temporomandibular arthropathies are the expression of a more generalized disorder that affects the entire stomatognathic system and can also involve other systems.
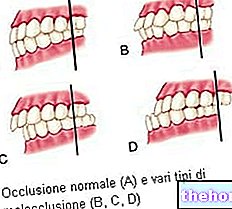
The most commonly encountered alteration is the intracapsular pathology which clinically begins with a small, sharp vibration or noise, more easily noticeable in the oral opening phase but also present in the closing phase which is defined, with an onomatopoeic term "click". The genesis of such disc-condylar incoordination is to be found in the anomalous dental match that triggers and supports the pathological mandibular posture by forcing the musculo-articular system into the best possible balance. The loss of this precarious balance in the joint and therefore the appearance of the full-blown pathology, will occur due to the exhaustion of personal adaptability and consequently to the failure of the support structures.It is in fact recurrent that the pathological dental occlusion occurs in forced mandibular retrusion with sliding back of the condyle and consequent stretching of the external pterygoid muscle and of the intra and extracapsular structures. However, from the prognostic point of view, the interception time of the joint problem is extremely important. which plays a dominant role in the evolution of anatomical damage very often painless, therefore underestimated. From a theoretical point of view, any alteration of the dental occlusion can lead to a morpho-functional degeneration of the temporomandibular joints; however, this particular clinical expression is commonly found in patients with significant losses of vertical dimension. Nevertheless, there are rare cases in which it is possible to verify a mandibular dislocation of modest degree, without loss of vertical dimension, but sufficient to generate the joint disorder. For this purpose, a 69-year-old woman was examined who complained of a slight noise in the left temporomandibular joint. The anamnesis also shows the presence of pain referring to the joint itself with irradiation to the homolateral ear. The symptoms appear to be of very recent onset, ie almost concomitant with the realization of a completed fixed prosthetic reconstruction of the second upper left premolar a few weeks earlier, by a colleague dentist Palpation of the articular regions reveals the presence of an opening click on the left joint with a modest pain in the retrodiscal tissues examined in maximum opening. No muscle pain was detected in the chewing and cervical muscles.
A computerized scan of the mandibular movements was performed to verify and measure, without interference from the operator, the presence of alterations in the usual pathways attributable to mechanical obstacles in the movement of the joint heads. This study was enriched by the simultaneous analysis in speed of the maximum opening movement of the mouth and subsequent closing. The assumption formulated is to analyze with sufficient precision any mandibular dislocations, deviations or deflections during normal movements almost always associated with inevitable slowdowns: the joint click must be considered a real obstacle anatomical which takes place when the dislocated articular disc is recaptured.The traces recorded in this way highlighted a maximum opening of 50.9 mm which occurs with a slight irregularity on the frontal plane in the intermediate phases of opening and closing.
The speed diagram, on the other hand, made it possible to clearly identify an average speed in opening of 267.6 mm / s and in closing of 260.0 mm / s with peaks over 400 mm / s. Less than 20 mm from the maximum opening, it is also possible to highlight an abrupt and short-term slowdown followed by a speed recovery which is reset when the jaw completes the opening phase and prepares for the next closing. it reappears in an almost specular way in the last millimeters of the closing path, near the dental contact that stops the movement.
A low-frequency preauricular TENS stimulation was then applied for 45 minutes with the aim of relaxing the stomatognathic and cervical muscles and identifying the neuromuscular trajectory that should be followed from the physiological resting position to achieve correct dental contact.
A new kinesiographic examination was therefore carried out to visualize the neuromuscular occlusion trajectory calculated following the path drawn by the mandibular movement that is achieved with the isotonic contraction evoked by electrical stimulation (TENS). This method is necessary in the first place to measure which is the patient's usual occlusion compared to the ideal one which should allow the arrest of the mandibular ascent along the same trajectory at a distance of 1.5-2.5 mm (physiological free space) from the position of mandibular rest.
In the case examined, the free space was found to be 1.4 mm but with a retruded position compared to the physiological one of 0.5 mm on the sagittal plane and aligned on the frontal one.
The presence of a physiological free space and the concomitant slight sliding backwards in maximum intercuspation led us to believe that the only intervention necessary was to remove from the dental surfaces those contacts that prevent the achievement of the myocentric position. This maneuver was rigorously carried out by evaluating not the usual contacts but the automatic ones induced by TENS stimulation adequately increased in intensity. The constant need not to interfere with the patient made us prefer the use of adhesive joint waxes rather than normal copying papers. In this way, those contacts on the cusp slopes usually avoided because they were judged harmful by the patient's proprioceptive system were identified. Once marked with a demographic pencil, they were reduced by coronoplasty in order to respect the height of the cusp and the depth of the pit but facilitating its entry and exit.
A new kinesiographic examination was then carried out on the same day which confirmed the correct respect of the vertical dimension previously measured and a substantial coincidence between the neuromuscular trajectory and the usual one traveled independently by the patient.
The patient was then checked at approximately one week and one month after the correction surgery and monitored remotely for a period of 6 months during which the individual Posselt diagram and the speed test were repeated.
The patient showed clinical signs of improvement during the first and only day of dental coronoplasty and already at the first check-up reported the disappearance of the painful symptoms with a notable reduction in joint noise which then completely disappeared after about 1 month.
The tracings carried out in the last visit show a better oral opening capacity both in a qualitative sense (reduction of irregularities on the frontal and sagittal planes) and in a quantitative sense (increase of the maximum oral opening). The speed test also shows how these movements take place without showing significant slowdowns in both the closing and opening paths.
All the parameters examined were decidedly more favorable than the respective ones recorded in the first visit and the patient confirmed the substantial benefit of correcting the dental surfaces by resuming the normal course of her activity previously compromised by non-stabbing but persistent pain. This aspect unequivocally describes the pathogenesis of the condylar disc incoordination: the dysfunctional picture of the neuromuscular system with involvement of the external pterygoid muscle in both heads must be connected to the ever present pathological mandibular posture. of the same fibers for the retroposition
condylar and the need to remodel the articular surfaces to ensure the functioning of the joint are the substrate in which all the pathogenic noxae that alter the dental coupling converge. If these assumptions are always present in the disc-condylar pathology, they cannot be considered sufficient since , as the patient well tells us you can live with these assumptions in full well-being as long as these tissues are able to resist stress. A direct mandibular trauma, an effort to maintain a protracted oral opening (wisdom tooth extraction), a slight further occlusal destabilization or even no apparent phenomenon may one day lead to the inability to bear further stress and therefore to determine the full-blown symptomatology that cannot be considered other than the onset of a problem that has taken root in the near past or remote articular logic represents only one side of a disorder that affects the entire stomatognathic apparatus and beyond. Unlike what was believed in the past, the joints cannot be considered dominant in the masticatory function but rather innocent victims when the complex intrinsic and extrinsic ligamentous system undergoes sometimes irreparable damage.