What is a Corneal Ulcer
A "corneal ulcer is a serious injury to the cornea, usually caused by an inflammatory process or an" infection.

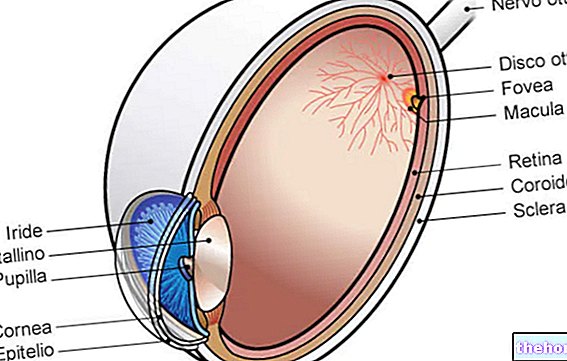
The corneal ulcer is similar to an open wound and is characterized by disruption of the epithelial (superficial) layer, with involvement of the stroma (deeper corneal layer) and underlying inflammation.
The symptoms of a corneal ulcer depend on the causes, size and depth of the lesion. The cornea is very sensitive, so even small abrasions can cause tearing, redness and pain. The corneal ulcer can be associated with hyperaemia and stratification of white blood cells in the anterior eye chamber (hypopion).
Treatment, usually based on topical antimicrobials, must be immediate to prevent complications and permanent damage; delayed or ineffective treatment of corneal infections can in fact lead to devastating consequences.
Causes
Corneal ulcers can be caused by trauma, chemical damage, misuse of contact lenses, corneal dystrophy, and keratoconjunctivitis sicca (dry eye). Other eye lesions are caused by eyelid abnormalities: entropion, exophthalmos, trichiasis and distichiasis (growth of the eyelashes in abnormal position and orientation).
Many pathogenic microorganisms are implicated in the "onset of" corneal ulcer. Among them are included bacteria (Staphylococcus aureus, Streptococcus viridans, Escherichia coli, Enterococci, Pseudomonas, Chlamydia trachomatis etc.), mushrooms (Aspergillus sp., Fusarium sp., Candida sp. and others), viruses (Herpes simplex, Shingles And Adenovirus) and protozoa (Acanthamoeba).

Common infections that can lead to the onset of a corneal ulcer are:
- Keratitis from Acanthamoeba:L"Acanthamoeba is a "unicellular amoeba, mainly present in soil and wastewater." Infection occurs mainly in contact lens wearers, most commonly due to exposure to contaminated water. Corneal ulcers from Acanthamoeba they are often intensely painful and may show transient epithelial defects and, later, a large ring-shaped infiltrate.
- Keratitis from Herpes simplex: it is a "viral infection that causes a" dendritic corneal ulcer which, over the course of an individual's life, can recur with recurrent attacks triggered by stress, exposure to sunlight or any other condition that weakens the immune system.
- Fungal keratitis: develops after an injury to the cornea most commonly caused by trauma with plant material, improper use of contact lenses or steroid eye drops. A fungal ulcer is deep but typically presents with slow onset and gradual progression; it is densely infiltrated and shows occasional small satellite lesions on the periphery. Fungal keratitis can also develop in people with weakened immune systems.
Non-infectious causes, any of which can be complicated by overinfection, include:
- Neurotrophic keratitis (resulting from loss of corneal sensation);
- Corneal exposure keratitis (due to inadequate closure of the eyelids, such as in the case of Bell's palsy);
- Severe allergic eye disease;
- Various inflammatory disorders, which can be exclusively ocular or part of a systemic vasculitis.
Other causes of corneal ulcers are: foreign bodies in the eye, abrasions on the ocular surface or nutritional deficiencies (especially vitamin A) € ‹. People who wear contact lenses, especially if they are soft, for a long period (including overnight), expired or not properly cleaned and disinfected, have an increased risk of developing corneal ulcers.
Superficial and deep ulcers
Ulcers are characterized by epithelial lesions of the cornea with underlying inflammation, which may soon progress to necrosis of the stroma. Superficial lesions involve a loss of part of the epithelium, while deep ulcers extend through the stroma and tend to heal with scar tissue, resulting in opacification of the cornea with decreased visual acuity. Uveitis, corneal perforation with prolapse of the "iris, pus in the anterior chamber (hypopion) and panophthalmitis (purulent inflammation of the eyeball) are consequences that can occur without treatment and sometimes even with the best available therapy, especially if medical intervention is delayed. Symptoms more serious and complications tend to occur with deep ulcers.
The location of the corneal ulcer may depend on the triggering cause. Central ulcers are typically caused by trauma, dry eye or corneal exposure from facial nerve palsy or exophthalmos. "Entropion, severe dry eye and trichiasis can cause a" peripheral corneal ulceration Immune-mediated eye diseases can cause ulcers at the border of the cornea and sclera, including rheumatoid arthritis, rosacea and systemic sclerosis. The latter, in particular, induces a particular type of lesion called Mooren's ulcer, which looks like a circumferential crater, usually with a protruding edge, as if it were a depression of the cornea.