
A rather complex operation, phalloplasty can be used in the presence of congenital defects of the penis (eg: micropenis, epispadias or hypospadias) or anatomical alterations of the penis, following traumatic events or the removal of a tumor; phalloplasty, moreover, is one surgical interventions offered to women who want to change their sex.
Modern phalloplasty involves the removal of a flap of skin from an area of the body usually hidden from view and the re-use of this skin flap in the construction, reconstruction or lengthening of the penis (this depends on the purpose of the procedure), and in the prolongation or remodeling of the urethra (even in this situation, everything depends on the purpose of the intervention).
Although it is safer than in the past and guarantees better results than a few decades ago, phalloplasty is still today an operation characterized by a not negligible risk of failure and complications.

- Men who, due to penile cancer, had to undergo the removal of a part of the organ affected by the neoplasm;
- Women who want to change their sex.
If in the first three circumstances (where the patient is a man) the phalloplasty corresponds to a "work of reconstruction / enlargement of the penis (in any case it is an intervention on an already existing organ), in the last one (where the patient is a woman) in a procedure of constructing a penis from scratch.
Two important notes about sex change phalloplasty:
- The phalloplasty for the change of sex from woman to man is the mirror intervention to the vaginoplasty for the change of the sex from man to woman.
- Phalloplasty for sex change should not be confused with metoidioplasty, which is the surgery for sex change from woman to man, preceded by a hormone therapy based on testosterone and characterized by the transformation of the clitoris into something much like a penis.

- A series of diagnostic tests, such as blood tests, electrocardiograms, urinalysis, etc., which are used to clarify the patient's state of health and ensure that the latter is suitable for undergoing surgery.
Pre-Operative Instructions for Phalloplasty: What to Do?
By pre-operative instructions s "means that" set of indications that a patient must have the foresight to follow, in the days preceding a certain surgical procedure.
In the case of phalloplasty, the pre-operative instructions consist of:
- Quitting smoking (this makes sense, of course, if the patient is a smoker). Cigarette smoking increases the risk of surgical incisions becoming infected; moreover, it alters the blood supply to the skin, which slows down the healing of the aforementioned incisions.
According to industry experts, smoking patients should initiate smoking cessation at least 2 weeks before surgery and implement it up to at least 2 weeks after the operation. - Temporarily stop, starting a few days before phalloplasty, any drug therapy that alters the normal blood clotting process (therefore, stop any treatments based on aspirin, warfarin, heparin, etc.).
- Present yourself, on the day of the procedure, on a complete fast for at least 8 hours. This means that, if the phalloplasty is scheduled in the morning, the last meal that the patient can take is the dinner of the day before the operation.
Fasting is part of the pre-operative instructions of any surgical procedure which involves general anesthesia or which, in particular circumstances, may require general anesthesia. - Ask a relative or close friend for their support on the day of the procedure, especially with regards to returning home once the operation is complete.
The use of a flap of skin including blood vessels and nerves is extremely advantageous, because it ensures the penis (both during construction, reconstruction or lengthening) the presence of blood circulation and nervous sensitivity (it will be task of the surgeon to connect the vessels and nerves in the new transplant site).
The extent of the removal (ie the size of the skin flap to be re-used for the penis) depends on the purpose of the phalloplasty: if the latter aims to build a penis from scratch, the skin flap to be removed will be larger , compared to what happens for a phalloplasty aimed at reconstruction or lengthening.
How does Phalloplasty in Women: some more details
The construction of a penis from scratch (therefore the phalloplasty aimed at changing the sex) is a much more complex and articulated operation than the reconstruction or lengthening of the penis (therefore the phalloplasty on a man), for the following reasons:
- Before phalloplasty, patients must undergo a long series of basic surgeries, such as: removal of large and small vaginal lips, removal of the vagina (vaginectomy), removal of the uterus (hysterectomy) and removal of the ovaries (oophorectomy);

- Except in special cases, during sex change phalloplasty the surgeon must:
- Create a sufficiently long tubular structure, which acts as a urethra (urethroplasty). This is explained by the fact that the female urethra is much shorter than the male urethra.
Urethroplasty is not a mandatory practice, in the sense that patients can still opt to keep the original urethra (in this case, they will continue to urinate while sitting); - Create, around the tubular structure that acts as the urethra, a second tubular structure, clearly larger, which has the appearance of a penis body. In this way, the surgeon has reproduced a real penis, with the urethra inside it. ;
- Join, through appropriate sutures, the neo-urethra and the neo-body of the penis to the patient's genital site;
- Rework the "innervation to the genital area, so that the neo-penis is provided with nervous sensitivity;
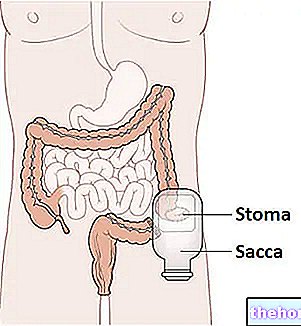
- Create a structure that, seen from the outside, acts as a scrotum (scrotoplasty) and, if the patient so desires, testicular prostheses (fake testicles) to be inserted inside. As a rule, for scrotoplasty, surgeons use the skin of the vaginal lips;
- To be able to count on a penis with erectile capacity, patients undergoing phalloplasty for sex change must undergo a "further surgical operation, aimed at the placement of a penile prosthesis (it is a kind of pump that allows the erection of the neo-penis ).
Curiosities about Phalloplasty for Sex Change
- The placement of the penile prosthesis can only take place once the surgical wounds, made for phalloplasty, have completely healed; this procedure, therefore, can only take place a few months after the phalloplasty.
- Some surgeons prefer to "break" the phalloplasty into multiple surgeries (eg, making the penis and urethra in one surgery and creating the scrotum in another surgery).
Phalloplasty: Surgical Techniques
To characterize a surgical technique for the execution of a phalloplasty is the site of the removal of the skin flap necessary for the intervention.
Currently, there are 4 surgical techniques useful for carrying out a phalloplasty:
- The technique that involves the removal of the skin flap from the radial forearm (phalloplasty with the radial flap of the forearm). It is the most recent technique and the one most performed, as the skin flap of the radial forearm ensures a high sensitivity to the penis;

- The technique that involves the removal of the skin flap from the lateral-anterior portion of the thigh (phalloplasty with the lateral-anterior flap of the thigh). It is a technique less and less used, as the lateral anterior flap of the thigh has a poor nervous sensitivity;
- The technique that involves the removal of the skin flap from the abdomen (phalloplasty with abdominal flap). It is the ideal technique for female patients who give up urethroplasty;
- The technique that involves the removal of the flap of skin from the skin area that covers the great dorsal muscle or latissimus dorsi (phalloplasty with musculocutaneous flap of latissimus backs). This technique is particularly useful when you need to build a penis within which a penile prosthesis can later be placed.
Phalloplasty: recovery after discharge
Upon returning home, the patient must rest from any physical activity for a period of time that can range from 4 to 8 weeks, depending on the complexity of the operation to which he has undergone (eg: phalloplasty for changing the sex involves a much longer period of rest from physical activity than is expected in the case of a reconstructive phalloplasty).
The first days following the operation are characterized by pain, bruises and burning in the surgery, by blood in the urine, by nausea and by the absence of nervous sensitivity at the level of the operated organ; with the passage of time, however, these disorders disappear: pain, bruises, burning and nausea disappear, the urine no longer contains blood and the transplanted skin flap is sensitive to touch.
To fully benefit from phalloplasty, during the first weeks following surgery, the patient must:
- Avoid applying pressure to the operated area;
- Try to keep the operated area elevated, to prevent it from swelling;
- Keep the operated area clean, according to the instructions of the attending physician. Cleaning is essential to avoid infections;
- Do not apply ice;
- Avoid taking a shower, unless otherwise indicated by the doctor (personal cleaning of the operated area must take place in other ways, which the doctor will exhibit in the appropriate locations);
- Empty the bag tied to the bladder catheter (if provided) at least 3 times a day;
- Do not pull on the bladder catheter (if applicable).
Did you know that ...
After a phalloplasty, the appearance of an appreciable nervous sensitivity in the area of intervention could occur even after many weeks.
excessive during surgery;Specific risks, on the other hand, include:
- Urethral fistula;
- Urethral stricture;
- Necrosis of the transplanted skin flap;
- Damage to the bladder or rectum
- Absence of nervous sensitivity.
The patients most at risk of complications are those undergoing phalloplasty for sex change, therefore female patients, due to the complexity of the procedure.













.jpg)











