Generality
The macula (or macula lutea) is a small region in the center of the retina, sensitive to light and responsible for sharp and detailed vision.

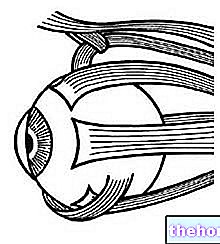
The human eye in cross section.
From: https://en.wikipedia.org/wiki/Macula_of_retina
The macula has some particular characteristics compared to the other retinal areas.It is, in fact, the region with the highest density of photoreceptors (in particular, cones), which are photosensitive nerve cells specialized in the transduction of light signals into electrical impulses, then interpreted by the brain as visual information (images).
The macula is an extremely delicate area and, for this reason, it is particularly vulnerable to pathological and degenerative phenomena.
Anatomy
The retina is the membrane that lines the innermost part of the eyeball. It adheres to the vascular tunic and is equipped with photoreceptors (cones and rods) and other neurons sensitive to light stimuli.
The ophthalmoscopic examination shows the retina as a red-orange colored lamina which presents, at the bottom - in a medial and lateral position with respect to the posterior pole of the eye - a small elliptical area, yellow-orange, of about 2-5 mm in diameter: the macula lutea.
Its center is laterally and lower than the optic disc (which coincides with the origin of the optic nerve). The macula has no blood vessels, which would obstruct the passage and capture of light.
Note. The yellow color of the macula, evident during the examination of the ocular fundus, is due to the presence of pigments belonging to the category of carotenoids, lutein and zeaxanthin. macular (in practice, carotenoids act as a kind of filter).
Fovea
The central portion of the macula is the fovea (or fovea centralis), a slight depression that represents the area of best visual definition. In the foveal region, the concentration of cones is maximum, while rods are completely absent.
Cones and rods
Cones and rods are specialized cells located in the outermost layer of the retina, capable of converting the light (physical) stimulus into an electrochemical signal to be sent to the brain. These photoreceptors do not have a uniform distribution: about 125 million rods form a "wide band around the retinal periphery, while in the posterior pole of the retina there are about 6 million cones, concentrated mainly in the macular region.
Their roles are also different:
- The rods allow black and white vision, are very sensitive to light and make it possible to see in low or low light conditions (scotopic or twilight vision).
- The cones are extremely different: there are, in fact, three types that perceive blue, green or red; their stimulation in various combinations allows the discrimination of different colors. Cones provide sharper and more defined images than rods, allowing you to see details, but require more intense light; they are mainly used in daytime vision.
Cones and rods consist of two parts: one has the task of capturing light, the other of adapting it to transmit it through the optic nerve fibers. Furthermore, each of these photoreceptors controls a certain portion of the retina: a visual image is, therefore, the result of the "elaboration of a" information transmitted by the entire receptor population.
Functions
The macula is the portion of the retina responsible for distinct vision (point) and color recognition, thanks to the maximum density of photoreceptors (mainly cones) and to the organization of nerve connections.
Point vision allows you to read, thread a sewing needle, recognize a face, see road signs while driving and distinguish details and very small objects. This explains why macular diseases have an immediate negative effect on visual function.
Contribution to vision
The macula is responsible for central vision (i.e. it allows us to focus our gaze at the center of the visual field, straight in front of us) and is more sensitive to clearly distinguish details than the rest of the retina. Here, in fact, the greatest amount of light rays are concentrated.
When we stare at an object, the emitted or reflected photons, after passing through the cornea, the pupil and the lens, are picked up by the cones of the macula. These photoreceptors are in relationship with a series of nerve cells present in the other retinal layers; their function consists in transforming light stimuli into electrochemical impulses, allowing them to be transmitted along the optical pathways, from the optic nerve to the brain.
Maculopathies
There are many diseases affecting the macula. Among these, hereditary and acquired forms are distinguished.

Macular involvement can also occur in systemic diseases, such as diabetes (diabetic retinopathy).
There are also maculopathies induced by the intake of particular drugs (for example, antimalarials, tamoxifen, thioridazine and chlorpromazine) or by post-operative complications (post-surgical cystoid macular edema).
Age-related macular degeneration
Age-related macular degeneration is the most frequent pathology of the macula and is the main cause of blindness after the age of 55 in developed countries. It is a chronic disease characterized by progressive changes in the retina, membrane of Bruch and choroid.
Age-related macular degeneration can evolve into two forms:
- Dry macular degeneration (atrophic): slow progression, it is the most frequent form (it concerns about 80% of cases). It begins with the formation of yellowish protein and glycemic deposits, called "drusen"; the reduction or disappearance (atrophy) cells of the macula, leads to a gradual decline in visual acuity.
- Wet macular degeneration (neovascular): faster in compromising vision, it is characterized by the growth of abnormal blood vessels from the choroid, in correspondence with the macula; Distortion of vision is caused by the leakage of blood and fluids from newly formed blood vessels, which collect under the macula and lift it. Wet macular degeneration is more aggressive than the dry form, as it can cause rapid and severe loss of central vision (caused by scarring of the blood vessels).
The causes of these maculopathies are not yet clear. However, several genetic, metabolic and behavioral factors have been identified that can increase the risk of macular tissue degeneration. These include cigarette smoking, prolonged exposure to intense sunlight, high blood pressure and high blood cholesterol levels. A balanced diet, rich in fruit and vegetables and low in animal fats, the abolition of smoking and periodic checks by the ophthalmologist are the most effective means to reduce the risk and catch the signs of the disease early.
Hereditary-degenerative macular dystrophies
Several less frequent forms of macular degeneration can begin in patients under the age of 55. Many of these early onset diseases are inherited and are more correctly defined as macular dystrophies.
Stargardt's disease (or juvenile macular dystrophy) typically begins in childhood and adolescence and is almost always inherited as an autosomal recessive trait. The progressive decrease in central vision associated with the disease is caused by the death of photoreceptor cells in the macula and by the involvement of the retinal pigment epithelium.
Other inherited maculopathies include late stage retinitis pigmentosa and Best's disease (or vitelliform dystrophy).
Myopic maculopathy
Myopic maculopathy occurs in people with degenerative or pathological myopia, a condition characterized by an increase in the axial length of the eye (greater than 26 mm) and a refractive defect greater than 6 diopters. Myopic maculopathy occurs for a series of anatomical alterations: the retina is unable to adapt well to the elongation of the bulb, therefore it undergoes strains or lesions in the periphery (small tears).
In pathological myopia, macular haemorrhages can occur with sudden decrease in visual acuity, sometimes with image distortion. The most fearful complication of myopic maculopathy is the subretinal neovascularization which, similar to what happens in age-related macular degeneration, causes subversion of the normal architecture of the macula and causes a severe loss of vision.
Macular pucker
The macular pucker consists of the development of a thin translucent membrane (called epiretinal) on the inner surface of the retina, above the macula. This sort of film can contract and lead to a wrinkling of the central area of the retina, altering its normal function.
Macular hole
The macular hole is a small break that affects the entire thickness of the retinal tissue and involves the foveal area.
This defect is associated with several pathological conditions: vitreo-macular traction (induced by the formation of epiretinal membranes), traumatic events, myopic degeneration, vascular occlusions and hypertensive retinopathy. Early symptoms of the macular hole include blurred vision, scotoma, and image distortion.
Symptoms of a Maculapathy
It is not always easy to notice the onset of a macular pathology, especially when it affects only one eye.
The main symptoms of a maculopathy include:
- Reduction of central visual acuity, with permanence of the peripheral one;
- Distortion of images (for example, straight lines may appear curved, objects appear offset in shape and size);
- Altered perception of colors, which appear faded;
- Decreased sensitivity to contrast;
- Presence of a "dark or empty area in the center of the visual field (scotoma)."
The central deformation of the image (metamorphopsia) is detected through the "Amsler grid", that is a pattern of perpendicular straight lines, on a black or white background, with a central point. During this simple evaluation, the patient covers one eye and stares the area in the center, keeping the grid 12-15 centimeters away from the face. With normal vision, all the grid lines around the point are straight, evenly spaced and without missing areas; if there is a distortion of the straight lines in the central visual area or a grayish spot appears that covers what is fixed, however, it is possible to suspect a disease involving the macula.
To evaluate macular function and check the state of the retina, then, it is essential to measure visual acuity and analyze the fundus with an ophthalmoscope. In order to correctly diagnose a maculopathy, the patient can also undergo instrumental examinations, such as "OCT (Optical Coherence Tomography), Fluorangiography and Indocyanine Green Angiography."













.jpg)











