Despite its small size, the thyroid performs fundamental functions for our health: thyroid hormones control metabolic activities and are responsible for the proper functioning of most of the body's cells. From the first weeks of life, the thyroid regulates development neuropsychic, body growth, metabolism, cardiovascular function, bone formation and growth. Not only that: it is always this gland that influences mood, muscle strength, fertility and more.
The thyroid tissue is organized into a large number of thyroid follicles, the walls of which consist of a single layer of follicular cells (thyrocytes). Inside the follicles there is a very viscous substance, the colloid, in which the synthesized hormones are accumulated and released from it, according to the needs of the organism. Finally, interleaved between the follicles are the parafollicular cells, responsible for the production of calcitonin, a hormone responsible for maintaining the balance of calcium in the body.
What does Endocrine Gland mean?
The thyroid is an endocrine gland: "gland" because it produces and releases hormones, "endocrine" because it releases its secretion into the bloodstream. Remember that hormones are "chemical messengers" that perform their biological function through different mechanisms of action. In practice, the endocrine glands transmit a specific "biological order" to the cells, releasing the hormones into the bloodstream, which act remotely. on target tissues Once the target is reached, the hormones exert their effect, eliciting responses and coordinating the various activities of the organism. Thyroid hormones are produced inside the follicles: thyroxine or tetraiodothyrosine (T4) and triiodothyronine (T3). The parafollicular cells, on the other hand, produce calcitonin.
(with internal secretion) located in the anterior region of the neck, in front of and lateral to the larynx and trachea. To put this into perspective, the thyroid is located at the level of the fifth cervical vertebrae of the spinal column, just above the base of the neck. The thyroid is bounded by a connective lamina adhering to the anterior and lateral surface of the trachea which allows it to move with swallowing.
Structure: shape, size and anatomical relationships
The shape of the thyroid resembles that of the letter H or of a butterfly with outstretched wings: it consists of two lobes, respectively right and left, placed on the sides of the larynx. The thyroid lobes are joined together by a sort of bridge that joins them, called the isthmus.
The thyroid is a very small gland: overall it measures only 5-8 cm in length and 3-4 cm in width. Its weight is quite variable and depends on some parameters, including nutrition, age and body constitution. In healthy adults, the weight of the thyroid gland averages around 10-20 grams, while in newborns it is around 2 grams.
Structurally, the thyroid is made up of a series of small, spherical vesicles called thyroid follicles. These circular cavities represent the functional units of the thyroid, that is, the smallest elements able to perform the functions to which this gland is responsible. The follicles have, in fact, the task of synthesizing, accumulating and secreting thyroid hormones. Precisely for this reason, each follicle is surrounded by a network of capillaries, into which the hormones produced are poured out when needed.
Thyroid follicles: characteristics and functions
Follicular cells or thyrocytes
The functional units of the thyroid are represented by the thyroid follicles. By examining in detail their structure, it is possible to notice that these have a spherical shape and are covered by a single layer of secretory cells, called follicular cells or thyrocytes. Thyrocytes delimit the follicular cavity containing the colloid, a viscous fluid with a high protein concentration. The follicular cells synthesize and pour into the colloid a globular protein rich in tyrosine residues, which acts as a precursor of thyroid hormones: thyroglobulin (Tg). Furthermore, in the follicular cavity there are enzymes for the synthesis of thyroxine (also called T4) and triiodiothyronine (or T3) and the iodide ion (I-, ionized form of iodine).
To be clear, the follicles could be compared to a series of "spherical bags" that act as both a "factory" and a "warehouse" for thyroid hormones.
The shape of the follicles depends on the functional state of the gland: when it is active and free the thyroid hormones in circulation, it has small follicles, almost empty of the colloid, and cylindrical thyrocytes; if, on the other hand, the thyroid is in a state of relative rest, then the follicles are bulky, the colloid is abundant and the thyrocytes are flattened.
Parafollicular cells or C cells
In the interstitial spaces between the follicles, there are parafollicular cells (or C cells), which synthesize and secrete the hormone calcitonin, involved in the regulation of plasma calcium concentration. In particular, the hormone inhibits the release of calcium from the bones ( hypocalcemic action) based on the plasma concentration of Ca2 + ions.
From the structural point of view, the parafollicular cells are independent and more voluminous than the thyrocytes and never access the follicular lumen.
Hormones
Thyroxine (T4) and triiodothyronine (T3)
Vascularization
As anticipated, the thyroid gland is a highly vascularized gland: the blood supply is guaranteed by the upper and lower thyroid arteries which give rise to a dense network of capillaries. A venous plexus that enters the internal jugular cells, on the other hand, guarantees the blood to flow back. from the gland.
. This amino acid is important because thyrocytes selectively take iodine from the blood and transport it to the follicular cavity, where it binds to the tyrosine of thyroglobulin to give rise to the thyroid hormones T3 and T4.
- Iodine is an essential trace element for thyroid function, as it is contained in both thyroid hormones; these hormones influence the activity of many organs and tissues, and have a broad spectrum of action on the metabolism of carbohydrates, fats and proteins and also on growth processes.
- In addition to iodine, it is important to remember that selenium also plays a key role in the functioning of the thyroid. It is no coincidence that the amount of this trace element in the gland is higher than in any other organ in the body. Selenium protects thyroid cells from oxidative damage and, at the level of target organs, participates in the reactions that activate thyroid hormones.
Returning to the characteristics of the thyroid follicles, it is important to note that the colloid is present inside them, which is a thick liquid with a high protein concentration. The colloid represents a sort of "warehouse" in which the thyroid hormones are stored and from where they are released according to the needs of the organism. For example, with exposure to cold, the thyroid releases its own hormones, which they act by increasing the basal metabolic rate, thus raising the oxygen consumption at the cellular level and the body temperature.
Thyroid hormones: T4 and T3
The hormones T4 (tetraiodothyrosine or thyroxine) and T3 (triiodothyrosine) regulate the body's metabolism and are necessary for the growth and normal development of the organism. T3 and T4 are produced by the thyroid follicular cells, in response to the modulation of TSH (stimulating hormone the thyroid).
Synthesis of Thyroid Hormones
Some elements are essential for the synthesis of thyroid hormones:
- Iodine;
- Tyrosine;
- Thyroperoxidase (TPO).
Iodine
Iodine is essential for the proper functioning of the thyroid, as it is present in the chemical structure of both thyroid hormones and plays a decisive role in controlling their production and release into the bloodstream. For this reason, it is very important to ensure a sufficient intake of the element, which occurs above all with the diet, ie through the consumption of certain foods, such as, for example, sea fish, crustaceans or products containing iodized salt. An insufficient intake. of iodine leads to an altered synthesis and reduced concentrations of thyroid hormones, which can cause various clinical manifestations. The best known consequence of iodine deficiency is goiter, ie the enlargement of the thyroid.
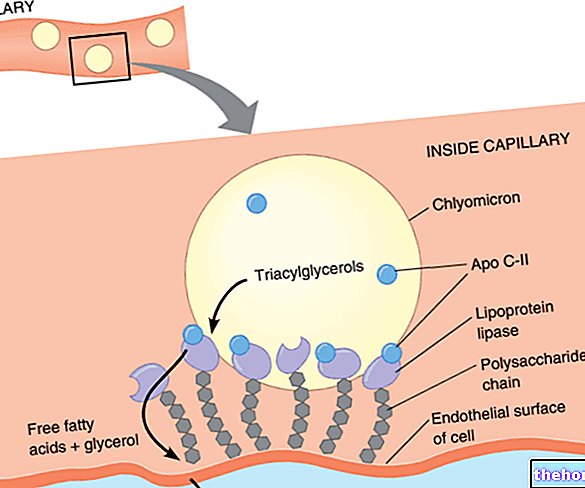
As for the synthesis of thyroid hormones, the iodine taken from the diet is absorbed in the intestine, is extracted from the plasma and concentrated in the follicular cells in the form of iodide (I-), with an active transport mechanism: the Na + symport / I- (NIS co-transports 2 sodium ions and 1 iodine against electrochemical gradient). The iodide captured by the thyroid is stored inside the colloid, where it is organized at I2 thanks to the thyroid peroxidase enzyme (TPO).
Tyrosine
In the colloid, there are also enzymes for the synthesis of T3 and T4 and thyroglobulin (Tg), which acts as a precursor for thyroid hormones. In fact, thyroxine and triiodiothyronine derive from the amino acid tyrosine and thyroglobulin (Tg) supplies the tyrosine residues necessary to form the skeleton of their chemical structure. All the components for the synthesis of thyroid hormones are therefore stored in the colloid.
Thyroperoxidase
The phases of the synthesis begin with the intervention of the enzyme thyroperoxidase (TPO), which catalyzes the iodination reaction of tyrosine: the addition of an iodide ion forms monoiodothyrosine (MIT) and the addition of a second iodide to the same molecule constitutes diiodotyrosine (DIT). MIT and DIT are nothing more than precursors of thyroid hormones: in fact, T4 derives from the condensation reaction between two molecules of DIT, while T3 is obtained from the condensation of one molecule of MIT and one of DIT.
The thyroid hormones thus formed are bound to thyroglobulin supports and are stored in the colloid before their release, for months after their formation.
Curiously, in fact, the thyroid is the only endocrine gland that possesses the ability to accumulate hormones in the extracellular area, before their release. When the TSH binding stimulates, in the follicular cells, the endocytosis of the thyroglobulin-thyroid hormone complex, thyroglobulin support is broken down by enzymes, while thyroid hormones are released into the cells, therefore into the bloodstream.
Feed-back of the synthesis of Thyroid Hormones

The synthesis and secretion of thyroid hormones are strictly regulated by very sensitive mechanisms. In particular, these are produced in response to the modulation of the thyroid hormone (or TSH, thyroid stimulating hormone), the release of which is stimulated by the release of the hypothalamic hormone TRH.
TSH is secreted by the anterior pituitary, a gland located at the base of the brain, and acts on follicular cells (or thyrocytes) by promoting the release of thyroxine and triiodothyrosine into the bloodstream.
TSH first binds to receptors on the follicular cell membrane, activating the second cyclic AMP messenger, and leads to the phosphorylation of a number of follicular cell proteins required for hormone secretion.
Thyroid hormones are subject to only small variations: their plasma levels are practically stable, since the main counter-regulation mechanism of the thyroid is negative feedback. In other words, the blood level of thyroid hormones controls the intervention of the hypothalamus and pituitary gland to limit the action of TRH and TSH (therefore high levels of thyroid hormones inhibit the release of TRH and TSH). thyroid hormones are kept within stable levels, which are defined as physiological, and which adapt to the different conditions of the organism.
Circulation and transport
- Through phagocytosis, thyroglobulin with annexes T4 and T3 is reincorporated into the lumen of the follicular cell and merges with a vesicle (lysosome). Inside this, T4 and T3 are freed from thyroglobulin by lysosomal enzymes, to be subsequently released into the bloodstream.
- T4 and T3 are transported into the circulation by plasma proteins: TBG (thyroxine-binding globulin), TTR (transthyretin) and albumin. A height, on the other hand, called FT4 and FT3 remains free and can reach the peripheral tissues.
- The circulating thyroid hormones are mainly represented by T4. Despite being secreted in lower quantities, in fact, T3 represents the most active form at the cellular level: it can be obtained through the desiodation of T4, which therefore represents a "prehormone". As a result, most of the plasma T3 is synthesized from T4.
- The activation reaction, i.e. the conversion of T4 into T3, occurs with the removal of an iodine atom, by the deiodases of type 1 (D1), type 2 (D2) and type 3 (D3).
- D1 is mainly expressed in the liver and kidney;
- D2 is mainly expressed in skeletal and cardiac muscle, central nervous system, skin, pituitary and thyroid;
- D3 is mainly expressed in the placenta, central nervous system and fetal liver.
- Thyroid hormones, once they reach their destination, are able to cross the plasma membrane, to bind to their receptor, present inside the target cells. The specific receptors for thyroid hormones, in fact, are found in the nucleus, where they can interact with DNA to regulate the expression of different genes.
Thyroid hormones contribute in a fundamental way to energy expenditure and to the endogenous production of heat, directly regulating the basal metabolism. This consists of the body's energy expenditure in conditions of rest and includes the minimum amount of energy necessary for the maintenance of basic vital functions, such as breathing, blood circulation and nervous system activities. If thyroid hormones increase, it accelerates the "metabolic activity in most tissues. The direct consequence is the increase in oxygen consumption and the speed of use of energy substances, with the production of heat, a phenomenon known as the thermogenic effect.
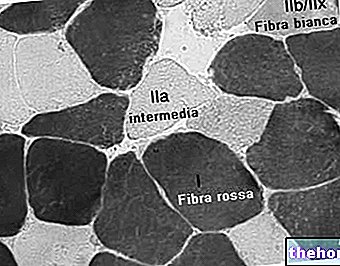
Part of this effect is due to the direct action of the hormones T3 and T4 on the mitochondria, the cell's energy plants. The thyroid hormones, in fact, stimulate the activity of some enzymes involved in oxidative phosphorylation reactions, at the level of the mitochondrial respiratory chain. , producing ATP and releasing energy in the form of heat.
T3 and T4 increase the metabolic activity of most of the body's tissues (exceptions to be noted are brain, spleen and gonads).
2. Effects on carbohydrate, lipid and protein metabolism
T3 and T4 not only intervene on the use of energy, but also on the mobilization of energy reserves, intervening in the synthesis and degradation of carbohydrates, lipids and proteins.
As regards glucose metabolism, these promote intestinal absorption of sugars, enhancing the action of insulin. At concentrations lower than normal, thyroid hormones stimulate gluconeogenesis in the liver and muscles, a process that converts glucose into glycogen or, on the contrary, if present in higher concentrations, they favor glycogenolysis, with a hyperglycemic effect.
In lipid metabolism, thyroid hormones are involved with different effects depending on their dosage. In case of thyroid hyperactivity, an increase in lipolysis may occur, with the depletion of the lipid deposit and an increase in the availability of fatty acids; vice versa, a deficiency of thyroid hormones causes the opposite effect, that is lipogenesis, with the synthesis of adipose tissue, which, among other things, leads to an increase in body weight.
Finally, thyroid hormones stimulate protein synthesis; however, if present in excess, they can cause the opposite effect, in the sense that they block protein synthesis and increase catabolism, ie proteins are converted into amino acids, often at the expense of muscle mass.
3. Effects on the cardiovascular system
Thyroid hormones have important effects on the cardiovascular system:
- They favor contractility and contribute to myocardial excitability;
- They increase the heart rate;
- Vascular resistance decreases, dilating peripheral arterioles and contributing to venous return.
All this has the purpose of guaranteeing the necessary oxygen supply to the tissues. To achieve this goal, the thyroid hormones can also determine an increase in pulmonary ventilation, which, to be efficient, requires an increase in cardiac output, that is the heart is made to pump more. From these effects also follows the increase in renal function.
4. Effects on the central nervous system
Thyroid hormones are necessary for the development of the central nervous system in the fetus and in the first weeks of life because they play a very important role in the differentiation and growth of nerve structures, as well as ensuring normal brain development. A deficiency of T3 and T4 in childhood can lead to a form of irreversible brain damage called cretinism, characterized by incomplete development of the central nervous system and mental retardation.. Thyroid hormones ensure correct synaptogenesis (growth of dendrites and axons) and myelination of nervous structures.
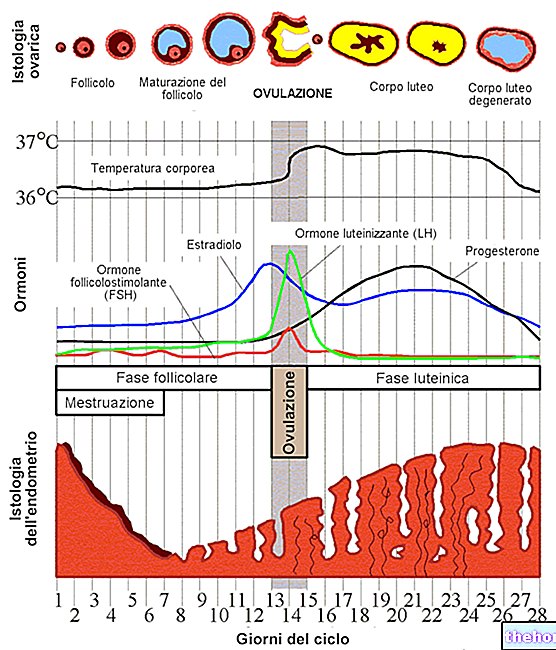
5. Effects on the reproductive system
Normal thyroid function is also important for the reproductive system. Thyroid hormones, in fact, influence the development and maturation of the testicles and ovaries, ensuring correct spermatogenesis and reproductive activity for men and the regularity of the menstrual cycle and the maintenance of pregnancy in women. A thyroid dysfunction can therefore cause consequences, such as infertility, sexual problems and menstrual disorders.
6. Other effects
Thyroid hormones:
- They increase intestinal motility;
- They favor the absorption of vitamin B12 and iron;
- They increase the synthesis of erythropoietin;
- They increase renal flow and glomerular filtration;
- They regulate the tropism of the skin and appendages;
- They stimulate the endogenous production of other hormones, including growth hormone or GH.
We can affirm that the thyroid hormones rather than intervening in a single site of action, modulate multiple and coordinated activities, allowing to maintain the normal physiological functions of the whole organism. Other specific biological effects vary from one tissue to another. It is worth adding that thyroid hormones are essential for the action of growth hormone or GH and produce sensitive effects on the musculoskeletal system, promoting bone remodeling and increasing muscle contraction capacity. Finally, many of the effects of stimuli on the metabolism are amplified by catecholamines, such as adrenaline and noradranaline, which act in synergy with thyroid hormones.
Calcitonin
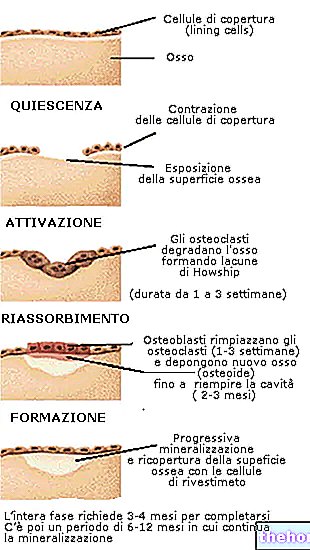
In addition to thyroid hormones, the thyroid also produces calcitonin, which is involved in the regulation of calcium metabolism. The hormone is synthesized and secreted by parafollicular cells or C cells in response to hypercalcemia, to contribute to the decrease in blood calcium concentration. Calcitonin lowers calcium through the inhibition of osteoclasts, therefore it promotes the deposit of calcium in the bone, and the stimulation of calcium excretion by the kidney. The antagonistic action is carried out by parathyroid hormone, the hormone secreted by the glands parathyroid glands.
it is a disorder associated with the hyperfunction of the thyroid gland, ie an excessive production of thyroid hormones; since thyroid hormones are responsible for controlling metabolism, hyperthyroidism causes an increase in many metabolic activities in the peripheral tissues. The most frequent symptoms are, in fact, weight loss, tachycardia, nervousness, tremors, insomnia, muscle weakness, increased sweating and intolerance to heat. Sometimes, the patient has very obvious signs, such as an enlarged thyroid gland and bulging of the eyeballs. The causes of thyroid hyperactivity are many. Hyperthyroidism can be, for example, the consequence of a hyperfunctioning thyroid nodule or Graves' disease, which consists of an autoimmune disease characterized by the production of autoantibodies that act like the TSH hormone, ie stimulating the thyroid.
Hypothyroidism
We speak, however, of hypothyroidism when the thyroid does not produce a quantity of thyroid hormones adequate to the needs of the organism. This can be due both to a "thyroid insufficiency, and to an" alteration of the balance between the thyroid, hypothalamus and pituitary , as, for example, in the case of an inappropriate secretion of TSH. This determines, in addition to the reduction of metabolic processes, symptoms such as fatigue, slowing of reflexes, reduced appetite and weight gain. The causes of hypothyroidism are different: iodine deficiency, autoimmune thyroid disease, outcomes of surgery and irradiation to the neck.
Goiter
Another condition is goiter, which defines, in a general way, any increase in the volume of the thyroid. gland. The increase in volume of the thyroid gland can occur both in cases of hyperthyroidism and hypothyroidism; bearing in mind that there are also goiters that do not modify thyroid function at all. In any case, the final result is the appearance of a bump on the neck, which it can even compress other nearby organs, making it difficult to swallow or breathe.
Thyroid nodules
The thyroid gland can also be affected by the formation of thyroid nodules. Their development is usually a benign phenomenon: often these small lumps localized on the thyroid, do not alter its functionality and do not cause any symptoms, but require a specific diagnostic evaluation, to exclude both tumor pathologies and possible future dysfunctions.
Tumors of the thyroid gland
Both benign and malignant tumors can arise in the thyroid. Thyroid tumors, with rare exceptions, often have a benign clinical course, therefore they can be controlled by therapy with excellent results.
Thyroiditis
Like all other organs, the thyroid gland can also be subject to inflammation. This possibility determines a picture of thyroiditis. The disease can have various causes, but the most common form is Hashimoto's thyroiditis, belonging to the group of autoimmune diseases. where an "abnormality of the immune system induces the production of antibodies against the cells of the thyroid itself.
Other articles on "Thyroid"
- Diseases of the thyroid gland
- Actions of thyroid hormones: thyroxine and triiodothyronine
- Thyroid hormones T3 - T4 and exercise
- Gozzigeni foods
- Thyroid and hormones, functions of the thyroid
Functions of the thyroid gland
Problems with playing the video? Reload the video from youtube.
- Go to the Video Page
- Go to Wellness Destination
- Watch the video on youtube
Related topics
- Thyroid hormones
- TSH
- Thyroglobulin
- Thyroiditis
- Thyroid goiter
- Blood Analysis: Thyroid Values
- Blood Thyroxine - Total T4, Free T4












.jpg)











