The intensity of pain that distinguishes dysmenorrhea is subjective and variable: for some women, the pain is light and barely perceptible, for others the intensity is such as to interfere with normal daily activities.
evident; in this case we speak of primary dysmenorrhea.In some cases, however, dysmenorrhea is the result of pathologies such as adenomyosis, endometriosis, fibroids, pelvic inflammatory disease (in these cases we speak of secondary dysmenorrhea).
Painful periods tend to subside after age 20 and may disappear after the first child is born.
in the lower abdomen, which often radiates to the lower back and thighs, diarrhea, nausea, sweating and dizziness.PLEASE NOTE
The information on drugs for the treatment of dysmenorrhea is not intended to replace the direct relationship between the health professional and the patient. Always consult your doctor and / or specialist before taking any type of medicine to counteract menstrual pain (even if freely available without a prescription).
are factors that can help keep menstrual pain under control. Furthermore, dysmenorrhea is perceived differently from person to person: if for some women it is perfectly bearable, for others the pain could be annoying and poorly tolerated or, in more serious cases, even hinder the performance of normal daily activities.
In such situations it may be useful to resort to the use of drugs, of course, on medical advice.
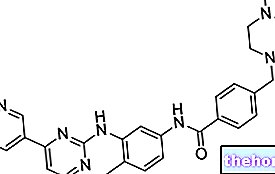
NSAIDs
In cases that require it, the pain typical of dysmenorrhea can be treated using oral non-steroidal anti-inflammatory drugs (NSAIDs). Ibuprofen and naproxen are among the most commonly used active ingredients in this sense.
These active ingredients are available in medicines that can also be dispensed without a medical prescription; however, it is advisable to always contact your doctor before taking them in order to identify any contraindications to the use of a given NSAID (for example, allergies to other types of non-steroidal anti-inflammatory drugs, other pharmacological therapies in progress, the presence of pathologies or conditions that may contraindicate the use of NSAIDs, etc.).
Hormone therapy
In particularly severe cases of dysmenorrhea, when pain makes it difficult to carry out even normal daily activities, the doctor may decide to prescribe hormone therapy with a low-dose estrogen-progestogen oral contraceptive to the patient. In this way, ovulation is suppressed and this could help reduce dysmenorrhea.
Other hormonal therapies, such as progestogen-only therapy or the use of intrauterine devices, can also be prescribed by the doctor in cases where he deems it necessary and useful for the patient.
Clearly, this type of drug can only be purchased upon presentation of a suitable medical prescription and, in any case, the start of hormonal therapy requires the evaluation of the doctor, or even better, of the specialist (gynecologist).
Non-drug treatment
Some useful tips for non-drug treatment of painful menstruation:
- Apply a bag of hot water to the level of the lower abdomen;
- Drinking hot liquids
- Consume light and frequent meals (delay meals in many small snacks);
- Practice relaxation techniques, such as yoga or meditation
- Take mineral and vitamin supplements (calcium, magnesium, vitamin B6) and, if the diet is deficient, supplement the diet with omega-three supplements (rich in EPA and DHA, such as fish oil);
- Lose weight if necessary and follow a regular exercise program;
- Practice a massage at the level of the lower abdomen.
Other Articles to deepen the topic
- Treatments and remedies for menstrual pain
- Menstrual pains - dysmenorrhea
- Herbal tea against menstrual pain