Bulimia Nervosa
Bulimia nervosa is an eating disorder (DCA) characterized by the fear of gaining weight and a strong desire to lose weight.
Typical attitudes of the bulimic include excessive food restriction and loss of control over food.
Discontrol results in binges and is followed by purgative methods, such as self-induced vomiting or the use of laxatives. Some practice motor compensation by carrying out excessively intense and / or prolonged physical activity (often fasting).

The causes are unclear and it is assumed that the pathological mechanism concerns the psychic and socio-cultural sphere. Bulimia nervosa is often affected by psychiatric comorbidities such as anxiety symptoms or disorders, depression, self-harm, and obsessive compulsive syndrome. Alcohol abuse and drug use are sometimes associated.
Complications related to bulimia nervosa are of various kinds.
Mentally, if left untreated, this condition can worsen and become chronic. Sometimes, it turns into anorexia nervosa.
As far as the physical aspect is concerned, bulimia does not necessarily cause excessive weight loss. On the contrary, cases of normal weight or overweight also seem frequent. This means that the risk of malnutrition is lower and less severe than for anorexia nervosa.
However, some complications related to compensation methods may be shown. Among these: dental or oral cavity diseases (for self-induced vomiting), intestinal disorders (for laxatives), metabolic problems (hypoglycemic peaks, hypotensive, fainting, etc.). muscle-articular (fatigue and excessive stress due to physical activity), specific vitamin and / or saline nutritional deficiencies.
Treating bulimia nervosa is difficult. It is based on the "multidisciplinary intervention that recruits four distinct professional figures: psychiatrist, psychologist, internist and dietician.
Dietary implications
The diet plan for bulimia nervosa does NOT have a curative value; in fact, it subordinates to an "adequate psychological therapy (eg behavioral therapy) and psychiatric (drugs).
The diet is however necessary to restore the nutritional balance and has a very important educational function. In particular, it helps the bulimic to rearrange the diet and acquire control over food, allowing him to manage the diet without leading to purgation / compensation. .
Before continuing, it should be noted that the treatment of bulimia nervosa is not easy. Most cases require several attempts; on the other hand, the perception of failure can aggravate the psychological condition.
Bulimics don't like to talk about their disorder. Typically, this confidentiality is caused by shame over one's behavior and sometimes one's appearance.
When bulimia nervosa creates a balance between binge eating and purging / compensating methods, allowing you to maintain weight, a difficult condition to “unblock” arises. Unfortunately, by hiding their behaviors, the bulimic delays the medical diagnosis by several months or even years compared to the appearance.
NB. Often, the bulimic hides the real goal of compulsive motor activity (weight loss), disguising himself as a competitive sportsman.
Characteristics of the Diet
ATTENTION! bulimia nervosa is NOT a condition that can be treated on its own. Consultation by specialists at specialized centers is recommended.
The diet for bulimia nervosa must show some indispensable characteristics, which concern the alimentary sphere and above all the psychic-behavioral one.
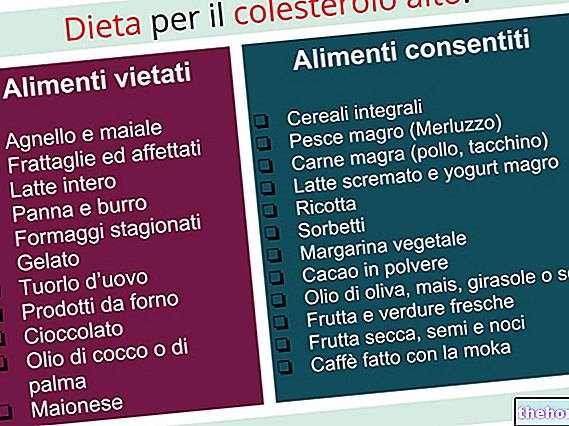
The table summarizes some of the fundamental elements for the diet of the bulimic subject.
EDUCATIONAL FEATURES
Norm-calorie diet. Bulimics should never be encouraged to lose weight, especially if they are of normal weight. The diet must meet all nutritional balance requirements.
Diet that guarantees NOT to gain weight. As anticipated, it is necessary to reduce stress, anxiety and the fear of gaining weight. It is possible to reduce the psychological causes of bulimic attacks by ensuring a diet that allows you to maintain weight.
In the case of severe metabolic disorders and obesity, a slightly low-calorie diet may be necessary. Keeping in mind the above, if the subject shows "evident obesity with metabolic pathologies, it may be necessary to promote weight loss. The decision is of medical interest (psychiatrist and internist).
Getting used to the feeling of hunger. It is typical of the prolonged fasts that follow binges. In the bulimic, the compulsive urge to eat has a much deeper root than the banal physiological stimuli.
Nonetheless, unaccustoming the patient's mind to perceiving the physiological impulses of hunger can greatly help in decreasing binges.
Variety. Alternate foods and try to consume at least one food for each basic food group. This is an aspect that, in the long term, favors the coverage of various nutritional needs. Furthermore, it allows us to dispel preconceptions of a dietary nature, often well rooted in eating disorders (for example, “pasta makes you fat”).
Avoid using food in conditions of anxious or depressive symptoms.
By eliminating the habit of consuming high-calorie foods when mood is compromised, feelings of guilt and the consequent means of compensation can be avoided.
It is interesting to note that anxiety predisposes to a greater consumption of salty and crunchy foods, while depression to sweet and creamy foods. However, during binges, the bulimic is not always fully aware of what and how much he is eating.
Supplements and drugs. If necessary, the bulimic should use over-the-counter medications or products to cover nutritional needs. The decision rests with the doctor and the dietician. For further information: Medicines for bulimia nervosa
Eat meals in company. Conviviality is a preventive factor for eating disorders. Eating in company is a very difficult correction to adopt because the subject feels the fear of losing control over food or fears of not being able to practice self-induced vomiting.
Non-aggressive attitude. The diet must be proposed with delicacy, established in common agreement and without impositions that could trigger an inevitable rejection.
Personalization. The diet for bulimia nervosa must be 100% personalized. Each case is unique, which is why there are no highly specific guidelines.















.jpg)











