Thyroid scintigraphy is a diagnostic imaging technique that provides valuable information not only on the morphology of this gland, but also and above all on its functionality. Like all scintigraphic techniques, it is based on the administration of radioactive drugs able to preferentially distribute themselves in the body area studied, in this case in the thyroid. The radiations emitted by the tissues made radioactive by the tracer are then picked up by a special receiver device, called gamma-camera and capable of detecting the emitted radiation (gamma rays similar to X-rays of radiographs).

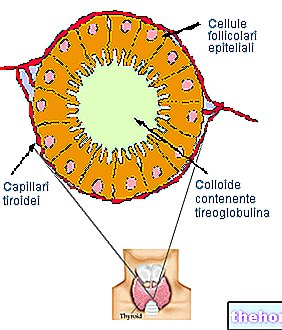
Since the thyroid is greedy for iodine, this being an essential mineral for the synthesis of its hormones, the classic tracer used in thyroid scintigraphy is radioactive iodine (123I and especially 131I), flanked by 99Tc; the latter - technetium 99 - is generally preferred both for its functional characteristics (shorter half-life) and for its low cost and lower irradiation.
In recent years, the diagnostic use of thyroid scintigraphy has been reduced in favor of ultrasound, which currently represents the first level investigation in patients with suspected thyroid pathology (it mainly provides information of a morphological nature). complementary survey, which among its most common indications recognizes:
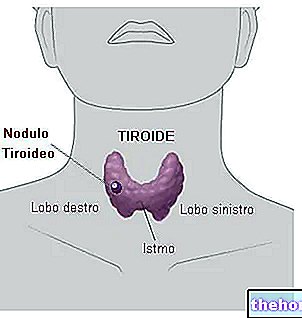
THYROID NODULES: small clusters of rounded cells, generally benign.
Thyroid scintigraphy allows to distinguish nodules already detected with other methods (ultrasound, palpation, etc.) in:
- hot (autonomously functioning, with risk of hyperthyroidism but mostly benign, see Plummer's adenoma);
- cold (with a reduced degree of activity compared to the rest of the gland, but with a greater probability of hiding a tumor; for this reason they often require a direct assessment by fine needle aspiration: with a fine, ultrasound-guided needle, samples are aspirated cells of the nodule, subsequently analyzed in the laboratory).
TOXIC MULTINODULAR GOZZO: hypertrophy and hyperplasia of circumscribed thyroid areas, variable in size, which become hypersecerning causing characteristic symptoms of hyperthyroidism. It differs from the so-called diffuse toxic goiter (Graves' disease), sustained by global thyroid hyperplasia.
THYREOTOXICOSIS: clinical picture that arises in response to the exposure of the tissues to the thyroid hormones present in excess; in this sense, thyroid scintigraphy helps the doctor to calculate the dose of Iodine 131 to be administered to the patient (in appropriate doses, this drug radioactive is also capable of destroying abnormal thyroid cells).
NEONATAL HYPOTHYROIDISM: search for thyroid agenesis (absence of the gland) or ectopic glandular tissue (i.e. external to the gland, such as lingual thyroid, struma ovarii, etc.).
PRESENCE OF METASTATIC THYROID TISSUE: in patients who have already undergone surgical removal of the gland (thyroidectomy), thyroid and total body scintigraphy is indicated to evaluate the presence of residual glandular tissue, possible relapses or metastases with preserved iodine uptake.
performing thyroid scintigraphy











.jpg)











