The plasma assay of protein S allows the identification of acquired and congenital deficiencies. A deficiency in this parameter can result, for example, from liver failure, anticoagulant treatment, vitamin K deficiency, estrogen-progestogen intake or high levels of estradiol for the " induction of ovulation.
which participates in the coagulation process: cooperating with other factors, this element has the task of counteracting thrombosis (understood as an "excessive coagulation activity), keeping the blood fluid. In other words, protein S is a physiological anticoagulant.For this reason, a "quantitative alteration or dysfunction of this anticoagulant protein represents a risk factor for thromboembolic events.
Protein S is synthesized in the liver and endothelial cells; its production is vitamin K dependent.
Variants of protein S: free form and bound form
In the bloodstream, protein S is present both in free (about 40%) and bound (60%) form:
- The free form of protein S is the ACTIVE variant and serves as a cofactor for protein C;
- The bound form of protein S is the INACTIVE variant; it is found in plasma in a form associated with the C4b binding protein (C4b carrier molecule, regulatory component of the complement system).
Coagulation: basic notions
Under normal conditions, after damage to tissues or blood vessel walls, blood loss is blocked thanks to "HEMOSTASIS. During this process, platelets adhere to the site of injury, so the reaction that leads to "activation of coagulation factors (coagulation cascade). This leads to the formation of a clot that remains until the damage is completely repaired. When it is no longer needed, this sort of "cork" is eliminated. The activity of protein S is expressed by favoring, as a cofactor, the action of another protein of the anticoagulant system: protein C.
Functions
Protein S is the main natural cofactor for protein C, activated in the proteolytic degradation of Factor V and Factor VIII. Protein S is therefore a physiological inhibitor of coagulation.
If there is not a sufficient amount of S and C proteins or these do not function adequately, clots can form uncontrollably. The consequences of this phenomenon can be mild or very serious.
Active Protein C, Protein S and Thrombin: biological role and blood coagulation
- Protein S and the active form of protein C (APC) cooperate for the formation of clots in the blood, controlling their extension, inactivating specific clotting factors (factor V and VIII).
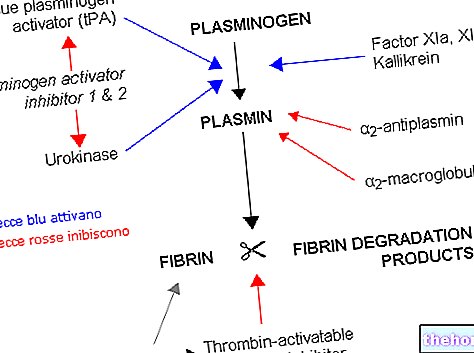
- In the presence of thrombin, generated by coagulation, and thrombomodulin, present on the endothelial surface, the C protein converts into the active form (note: this factor does not enter anything with the C reactive protein). Thanks to this structural modification, the active protein C also acquires a pro-fibrinolytic activity (it favors the dissolution of the clot), which it carries out through the inhibition of PAI-1 (inhibitor of the plasminogen activator).
- It should also be remembered that thrombin (coagulation factor IIa) converts fibrinogen into an insoluble fibrin polymer, which participates in the formation of the clot. This pro-coagulant action of thrombin contrasts with its ability to activate protein C; the phenomenon therefore represents a form of endogenous control over the excessive activity of the coagulation system.
To evaluate protein S, two types of tests are available:
- Functional examination: measures the activity of protein S, focusing on the ability to regulate and decrease the formation of clots. The decrease in activity may be due to a reduced quantity of the parameter or to the presence of non-functional forms.
- Immunological analysis: establishes the amount of protein S present in the blood sample taken from the patient (note: the amount of free, bound or total protein S can be measured with this test).
This information can be useful in determining the type and severity of S protein deficiency.
When is the exam prescribed?
The examination of the coagulation protein S allows to measure its quantity and evaluate its functionality.
This analysis is generally indicated after an unexplained thrombotic event, as an aid to the diagnosis of hypercoagulation disorders, especially in young subjects (less than 50 years of age) and / or who have no other obvious reasons for this phenomenon. .
Protein S testing may also be required for multiple miscarriages. Furthermore, it is very important to check the values of this protein before taking oral contraceptives; in women at risk, estrogen and progestogen drugs could cause venous thrombosis or other cardiovascular disorders.
Evaluation may also be advised when a patient has a close family member with an inherited S protein deficiency.
Related exams
In association with the protein S test, the doctor may also indicate that the following tests are performed:
- Coagulation protein C;
- Antithrombin III;
- Mutation of coagulation factor V;
- Mutation of coagulation factor II;
- Homocysteine.
Congenital or acquired protein S deficiencies result in hypercoagulability (or a prothrombotic state).
Protein S: acquired defects
Acquired protein S deficiency may be due to:
- Reduced synthesis;
- Increased consumption;
- Loss or passage of protein S from free to bound form.
The acquired protein S defect can be associated with:
- Liver diseases (cirrhosis, liver failure, chronic hepatitis, etc.);
- Excessive consumption (as in disseminated intravascular coagulation);
- Vitamin K deficiency (reduced or missed dietary intake, therapies with dicumarolics or antibiotics that interfere with the synthesis of this vitamin, etc.);
- Post-operative states;
- Therapy with coumarin anticoagulants;
- Severe or chronic infections;
- Acquired Immunodeficiency Syndrome (AIDS);
- Pregnancy;
- Taking oral contraceptives;
- Acute syndromes characterized by suffering of the respiratory system;
- Inflammatory bowel disease;
- Kidney disease (nephrotic syndrome, renal dysfunction;
- Systemic lupus erythematosus;
- Diabetes;
- Heart attack;
- Oncological diseases.
Often, in these acquired forms, the other natural anticoagulants, such as antithrombin III, are also decreased.
Protein S: congenital deficiencies
Congenital deficiencies of protein S can be caused by:
- Reduced synthesis;
- Synthesis of proteins with reduced biological activity (dysfunctional) for:
- Reduced ability to bind to protein C;
- Reduced degradation capacity of factors V and VIII.
Hereditary protein S deficiencies are classified into three types:
- Type I deficiency: there is a decrease in free protein S levels, while the total protein S is normal or slightly reduced (quantitative defect);
- Type II deficiency: functional activity of the protein decreases, but the free protein S values and total protein S levels are normal (qualitative defect).
- Deficit type III: it is a quantitative deficiency, in which there is a decrease in the levels of free protein S and normal levels of total protein S (quantitative defect).
Low protein S: possible consequences
Protein S deficiency is generally associated with an increased risk of thromboembolic events.
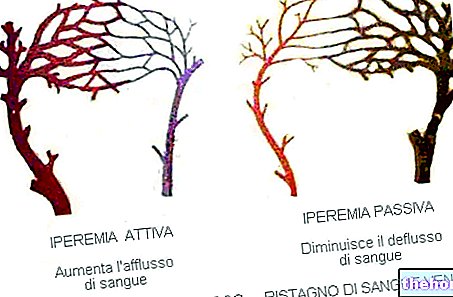
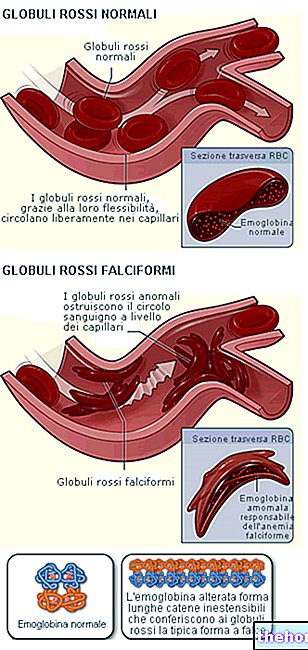
A deficiency of protein S translates, in fact, into a reduction in the anticoagulant activity of the blood (or in a state of thrombophilia); consequently, the risk of abnormal clots (the so-called thrombus) forming in the blood vessels increases.
These "lump" like formations can:
- Go towards spontaneous dissolution;
- Grow to the point of obstructing the vessel in which they originate;
- Break, migrating into a circle and sometimes ending up occluding a smaller vessel.
The most fearful consequences of this condition, called thrombosis, are heart attack, stroke and pulmonary embolism. Protein S deficiency is the underlying cause of a small percentage of cases of disseminated intravascular coagulation (DIC) and thrombosis. deep vein (DVT).











.jpg)











