Generality
Arnold-Chiari syndrome is a set of signs and symptoms caused by a rare malformation of the posterior cranial fossa; in subjects affected by it, this structure is not very developed, so the cerebellum exits (protrudes) from its natural site through the foramen magnum, located at the base of the skull.

There are four different types of Chiari malformation; the parameter that distinguishes one type from another is the degree of protrusion, therefore the amount of cerebellar material involved. Type I is the least severe (sometimes it remains asymptomatic for life), while type IV is the most severe; however, starting from type II, the quality of life is compromised.
Symptoms that characterize Arnold-Chiari syndrome are numerous and range from headache to muscle weakness etc.
To date, there is no cure that allows to repair the cerebellar malformation, however there are treatments that allow to alleviate, at least in part, the symptoms.
What is Chiari malformation
Chiari malformation, or Arnold-Chiari syndrome or even more simply Arnold-Chiari, is a "structural alteration of the cerebellum, characterized by a downward displacement, precisely in the direction of the occipital foramen and the spinal canal, of the portion baseline of the cerebellar hemispheres.
In other words, it is a "cerebellar hernia, in which part of the cerebellum protrudes from the foramen magnum invading the spinal canal.
WHAT IS THE OCCIPITAL FORUM?
The foramen magnum, or foramen magnum, is a large opening located in the lower part of the occipital bone of the skull. This hole connects the spinal canal with the cranial cavity. ) first the medulla oblongata and then the spinal cord.
Fundamental joint for the circulation of the cerebrospinal fluid (or liquor), the foramen magnum is crossed by the vertebral arteries and by the anterior and posterior spinal arteries.
ORIGIN OF THE NAME
Arnold-Chiari syndrome takes its name from the two doctors who first described it, Julius Arnold and Hans Chiari.
It is not to be confused with Budd-Chiari syndrome, which is a morbid condition affecting the liver.
Causes
Based on the severity of the protrusion and the time of life in which it originates, the Chiari malformation can be divided into 4 different types, identified by the first four Roman numerals (I, II, III and IV).
The first two types, when compared to the second two, are more common and less severe; type III and type IV, in fact, are very rare and incompatible with life.
MALFORMATION OF TYPE I CHIARI
Chiari type I malformation is asymptomatic (ie without obvious symptoms), at least until childhood or late adolescence.
Its cause of origin is to be found in the reduced cranial space: in such conditions, in fact, a part of the cerebellum (precisely the cerebellar tonsil or tonsils located on the lower side), is forced, due to lack of space, to slip into the foramen magnum and enter the spinal canal.
Attention: Several people with type I Chiari malformation are doing well and leading completely normal lives. This is due to the fact that the cerebellar anomaly is not so severe as to cause symptoms or disturbances. Therefore, very often, such people ignore their condition or become aware of it by chance.
MALFORMATION OF TYPE II CHIARI
Type II Chiari malformation is a congenital disease, that is present from birth, and always symptomatic.
Compared to type I, it is characterized by a greater protrusion, which in addition to the cerebellar tonsils also involves a portion of the cerebellum (called the cerebellar vermis) and a venous vessel known as the Herophilus torcularis.
Most often, Arnold-Chiari type II is associated with a particular form of spina bifida called myelomeningocele.
Among the various consequences of this malformation, we note: the blocking of the flow of liquor through the foramen magnum (which leads to the onset of a condition called hydrocephalus) and the interruption of nerve signaling.
Initially, the term Arnold-Chiari referred only to Arnold-Chiari type II syndrome. Now, it is commonly used for all forms of the disease.
MALFORMATION OF TYPE III CHIARI
Present from birth, type III Chiari malformation causes severe neurological problems, so much so that it is often incompatible with life. In these cases, in fact, the protrusion of the cerebellum is marked and for this reason we speak of occipital encephalocele.

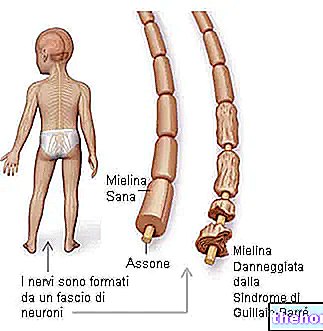
Figure: syringomyelia.
From the site: mdguidelines.com
Usually, Arnold-Chiari type III is characterized by hydrocephalus and syringomyelia; the latter represents a particular condition, characterized by the presence of one or more cysts inside the spinal canal.
MALFORMATION OF TYPE IV CHIARI
Chiari malformation type IV is characterized by the failure of part of the cerebellum to develop (cerebellar agenesis).
This anomaly is congenital and absolutely incompatible with life.
ASSOCIATED DISEASES
Doctors and scientists have observed that the following conditions are also common among individuals with Chiari malformation:
- Hydrocephalus
- Syringomyelia
- Stiff spine syndrome
- Severe curvature of the spine
- Marfan syndrome
- Ehlers-Danlos syndrome
IS IT AN HEREDITARY DISEASE?
Researchers believe that the Chiari malformation may have a "hereditary origin, as some recurrence has been reported in the family.
However, the genetic conditions that cause the appearance of the disease (i.e. which and how many genes are involved) and the type of transmission remain to be clarified.
EPIDEMIOLOGY
The precise incidence of Chiari malformation is unknown; this is because several people with Arnold-Chiari type I do not experience any symptoms and appear completely normal (therefore the disease is underdiagnosed).
The few reliable epidemiological researches report that:
- Type I is symptomatic in one in 100 children
- Type II is particularly widespread in populations of Celtic origin
- Women are 3 times more affected than men
Symptoms and Complications
The 4 types of Chiari malformation have different symptoms and signs.
Below is an accurate description of the symptoms that characterize types I, II and III.
For type IV, it is impossible to trace a symptomatology, as it is a condition that inevitably and suddenly leads to the death of the fetus.
MALFORMATION OF TYPE I CHIARI
When type I Chiari malformation is symptomatic, it can cause:
- Severe headaches, the onset of which is frequent after coughing, sneezing and overexertion.
- Pain in the neck and / or face
- Problems with balance
- Frequent dizziness
- Problems speaking, such as hoarseness
- Vision problems, such as double or blurred vision, pupillary dilation and / or nystagmus
- Difficulty swallowing (dysphagia) and chewing
- Tendency, when eating, to suffocation
- He retched
- Sense of numbness in the hands and feet
- Lack of motor coordination (especially in the hands)
- Restless Legs Syndrome
- Tinnitus (or tinnitus), ie the hearing disorder for which one has the sensation of perceiving, in the ear, non-existent noises, such as rustling, buzzing, whistling, etc.
- Sense of weakness
- Bradycardia. It is the medical term for a slowing of the heart rate
- Scoliosis associated with spinal cord disorders
- Abnormal breathing, especially during sleep (sleep apnea syndrome)
MALFORMATION OF TYPE II CHIARI
Type II Chiari malformation is characterized by the same symptoms as type I, with the difference that these have a more marked intensity and are always present. Furthermore, if accompanied by myelomeningocele, type II Arnold-Chiari also causes:
- Intestinal and bladder alterations: the patient loses control of the anal and bladder sphincters
- Convulsion
- Extremely developed corpus callosum
- Extreme muscle weakness and paralysis
- Deformity in the pelvis, feet and knees
- Difficulty walking
- Severe scoliosis
Spina bifida and myelomeningocele
Spina bifida is a congenital malformation of the vertebral column, due to which the meninges, and sometimes also the spinal cord, come out of their seat (they are normally confined to the inside of the vertebrae).
Myelomeningocele is the most severe form of spina bifida: in those affected, meninges and spinal cord protrude (or hernian) from their vertebral housing and form a protruding sac at the level of the back. This bag, although protected by a layer of skin, is exposed to external insults and is continuously at risk of serious infections and, in some cases, even fatal.
MALFORMATION OF TYPE III CHIARI
People with type III Chiari malformation suffer from severe neurological problems (often incompatible with a normal life), hydrocephalus and syringomyelia. The latter, characterized by the formation of one or more cysts inside the spinal cord, can be the cause of:
- Muscle weakness and atrophy
- Loss of reflexes
- Loss of sensitivity to pain and ambient temperature
- Stiffness in the back, shoulders, arms and legs
- Pain in the neck, arms and back
- Bowel and bladder problems
- Extreme muscle weakness and leg spasms
- Pain and numbness in the face
- Scoliosis
WHEN TO SEE THE DOCTOR?
Chiari malformations of type II, III and IV are already visible in the prenatal age (ie when the affected subject is still in the maternal uterus), through an ultrasound examination.
As regards, instead, the Chiari malformation type I, it is advisable to consult a doctor as soon as the typical symptoms reported above appear. It is important to undergo timely checks also because other associated disorders may emerge from the latter.
COMPLICATIONS
The complications of the Chiari malformation are linked to a worsening of the cerebellar protrusion or to the associated morbid states, therefore to hydrocephalus, myelomeningocele, syringomyelia, rigid spine syndrome, etc.
The worsening of the protrusion, which is due to a greater pressure of the skull to damage the cerebellum, obviously implies an aggravation of the symptoms.
Diagnosis
The diagnostic tests that allow to establish the degree of protrusion of the cerebellum through the foramen magnum (thus establishing the type of Chiari malformation) are:
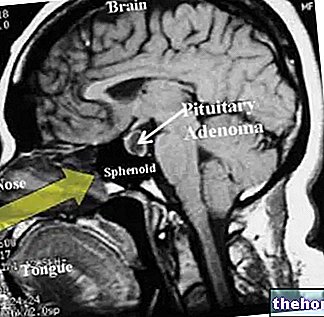
- Nuclear magnetic resonance (or MRI). Thanks to the creation of magnetic fields, it provides a "detailed image of the cerebellum and spinal canal, without exposing the patient to harmful ionizing radiation.
- CT scan. Computed tomography (CT) provides clear images of internal organs, including the cerebellum and spinal cord. During its execution, the subject is exposed to a minimal amount of harmful ionizing radiation.
CT and MRI, preceded by an accurate physical examination, are essential to identify any pathologies associated with Arnold-Chiari.
Table. How and when to diagnose Chiari malformation.
When and how can it be diagnosed?
THE
Late childhood or late adolescence, with a physical examination followed by CT and / or MRI.
II
In the prenatal age, with an "ultrasound.
At birth and very early infancy, with a physical examination, CT scan and / or MRI.
III
In the prenatal age, with an "ultrasound.
At birth with a physical examination, CT and / or MRI.
IV
In the prenatal age, with an "ultrasound.
Treatment
Chiari malformation is incurable.

Sagittal scan obtained by FLAIR MRI, showing an Arnold-Chiari malformation with 7 mm herniated cerebellar tonsils. From the site: en.wikipedia.org
However, there are both pharmacological and surgical treatments, which allow to alleviate, at least in part, the symptoms.
PHARMACOLOGICAL THERAPY
Chiari type I patients who suffer from headache and neck and / or face pain may take pain medication.
The choice of the most suitable medicines for each individual case is up to the attending physician; therefore, it is good practice to follow its prescriptions.
SURGICAL THERAPY
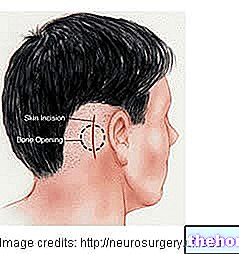
The goal of surgical treatment is to reduce the compression exerted by the skull on damage to the cerebellum and spinal cord.
To achieve this, there are several procedures, such as:
- Decompression of the posterior fossa, during which the surgeon removes part of the posterior portion of the occipital bone.
- Decompression of the spinal cord, using a laminectomy (or decompressive laminectomy). During its execution, the surgeon removes the lamina of the second and third cervical vertebrae. The lamina is the vertebral portion that delimits the hole through which the spinal cord passes.
N.B: Sometimes, posterior fossa decompression and decompressive laminectomy are performed simultaneously. - The decompressive incision of the dura mater. With the incision of the dura mater, or the outermost menynx, the space available to the cerebellum increases and the pressure against it decreases. To cover and protect the gap created by the incision, the surgeon sews a piece of artificial tissue (or collected from another part of the body) over it.
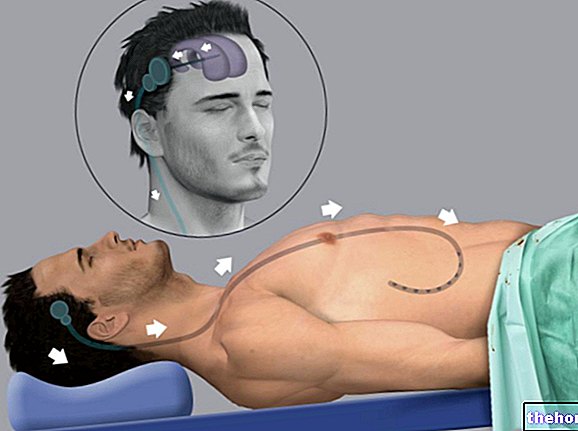
- The shunt surgical. It is, in fact, a drainage system, consisting of a flexible tube that allows the elimination of the liquor, in the case of hydrocephalus, or the emptying of the cyst or cysts, in the case of syringomyelia. It is possible that patients with hydrocephalus have to do use of shunt surgical for life.
RISKS OF THE SURGICAL INTERVENTION
The risks associated with surgery are different. It is possible, in fact, that there are: hemorrhages, damage to the brain structures and / or the spinal cord, infectious meningitis, problems with wound healing and, finally, unusual collections of fluid around the cerebellum.
It should be remembered that any brain or spinal cord damage, which occurred during the surgery, is irreparable.
Therefore, before undergoing any type of surgery, the operating doctor will expose any risks and complications of the necessary procedure or procedures.
Prognosis
Chiari malformations type II, III and IV never have a positive prognosis, as, in addition to being incurable, they can cause severe neurological deficits or even be incompatible with life.
The case of type I Chiari malformation is different, the prognosis of which varies according to the severity of the symptoms.