According to the "American Dental Association (American Dental Association), gingivitis is, together with periodontitis, the main cause of tooth loss in adults.
) favored by poor oral hygiene: in fact, bacterial plaque (or dental plaque) formed on the teeth and not adequately eliminated by brushing, and its subsequent calcification into tartar are often responsible for the inflammatory process of the gums.
Formed by food residues, bacteria and mucus, and favored by poor oral hygiene, the plaque tends to calcify, turning into tartar; the increase of these particularly hard deposits, impossible to remove with normal home oral hygiene practices, together with bacterial activity, determine an irritative process characterized by symptoms of various kinds, such as swelling and inflammation of the gums themselves.
Much more rarely, gingivitis is the result of traumatic insults affecting the gum itself, caused for example by too vigorous brushing.
The presence of bacterial plaque is also responsible for the formation of dental caries.
For further information: Dental Plaque (or Bacterial Plaque)Gingivitis: the Risk Factors
Risk factors for gingivitis include:
- Poor oral hygiene;
- Smoking, due to the toxic substances contained in it, and, for the same reason, the chewing of tobacco;
- The advanced age;
- Pregnancy and puberty, due to the strong hormonal fluctuations that characterize these particular periods of life;
- Diabetes;
- The genetic predisposition;
- The stress;
- Conditions that lead to a weakening of the immune defenses (immunosuppression), such as for example AIDS, leukemia and cancer treatments;
- Malnutrition, in particular when it leads to vitamin deficiencies (eg vitamin C);
- The use of certain drugs, including some antihypertensives, cortisones, antidepressants and antiepileptics, as they can increase the volume of the gums and, in this way, negatively affect oral health.
Acute Ulcerative Gingivitis Necrotizes: the Causes
An uncommon but particularly severe form of gingivitis is the so-called acute ulcerative necrotizing gingivitis, which manifests itself in an acute form with fever, ulceration, marked halitosis and intense pain.
This condition arises above all in debilitated patients and is due to the synergistic infection of specific anaerobic microorganisms.
In an advanced stage, inflammation is accompanied by more severe symptoms; spaces between the teeth, gingival recessions with exposure of the roots and excessive tooth mobility may appear.
For further information: Gingivitis SymptomsGingivitis: when to go to the dentist?
In the presence of symptoms such as gingival bleeding, bad breath and change in the appearance of the gums, it is advisable to promptly contact your dentist in order to assess the problem and receive information on the remedy to be taken.
On the other hand, it is not advisable to spontaneously use mouthwashes or special toothpastes, without first consulting a specialist, which, if the wrong type or in excessive doses, can be harmful.
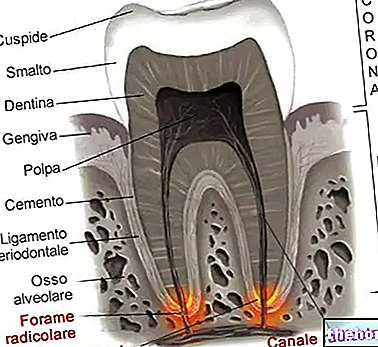
, periodontosis or periodontal disease; the latter, as the name suggests, affects the periodontium, that is the set of structures surrounding the tooth (the gum, the bone that supports it, the cementum of the root and the ligament that holds it anchored to the bone) .Gingivitis: how does it evolve into periodontitis?
If neglected and not treated, gingivitis involves a retraction of the normal gingival sulcus, to form - with the complicity of the bacterial plaque that generated it - the so-called periodontal pockets.
The term "pockets" perfectly describes what periodontal pockets are: they are anomalous spaces that open between the teeth and the gum wall that usually adheres to the teeth themselves.
The periodontal pockets represent a problem, because the bacteria of the dental plaque can accumulate in them undisturbed; undisturbed, as the abnormal space between tooth and gum is unreachable by saliva (which could act as an antibacterial substance) and drugs.
In the long run, the accumulation of plaque in the periodontal pockets causes the bacteria to creep more and more towards the bones that support the teeth (periodontitis); once they reach the bones at the base of the teeth, the bacteria also affect these, up to cause mobility of the teeth themselves and, in extreme cases, their fall.
Unfortunately, the whole process described above often occurs asymptomatically, so much so that periodontal disease can progress and worsen almost without realizing it.
For further information: Periodontitis: Causes and Remedies, in order to establish the state of health of the bone that supports the teeth.Gingivitis Diagnosis: Understanding the Cause
To understand the reasons for gingivitis, the medical history is very important; in fact, through questions relating to diet, lifestyle habits (eg: smoking), the frequency of tooth brushing and how the teeth are brushed, the dentist is able to trace the probable triggers of gingival inflammation.
is mainly based on the practice of good oral hygiene, which includes both the use of toothbrushes and dental floss, and on the elimination of all those causal and risk factors associated with the inflammatory disorder (for example, if the patient is a smoker, should stop smoking).For further information: Remedies for Gingivitis
Gingivitis: How to Brush Your Teeth

Proper oral hygiene includes:
- Brushing teeth 2-3 times a day; very important is washing before going to bed.
Teeth brushing must be done correctly: from top to bottom and never horizontally or from bottom to top.
A very effective toothbrush in removing plaque is the electric one: it involves a small economic investment, but, if well preserved, it lasts over time and guarantees excellent results. - The use of dental floss and, if necessary, the brush. Also the use of dental floss must be done with the right technique, in order to avoid damaging the gum.
- The use of quality toothpastes.
Gingivitis treatment: the role of the dentist
If the gingivitis is severe or has already resulted in the formation of tartar, the intervention of the dentist with a professional oral hygiene is necessary.
In these situations, the role of the specialist is fundamental for at least two reasons:
- Because tartar is not removable with a normal toothbrush or dental floss, e
- Because the dentist has tools with which he is able to eliminate bacterial plaque even from the most uncomfortable and difficult to reach points, all without causing damage to the gum.
Furthermore, it must be remembered that professional oral hygiene intervention allows the dentist to clearly observe the teeth and identify any caries.
Gingivitis Treatment: Use of Mouthwash
In some cases of gingivitis, the dentist may indicate the use of an antiseptic mouthwash (usually based on chlorhexidine).
Antiseptic mouthwashes help control bacterial plaque. However, they are not a substitute for toothbrush and dental floss, which are always the remedy of choice for the elimination of bacterial plaque; moreover, their prolonged use can alter the natural color of the dental enamel.
Finally, we remind you that the use of mouthwashes should only be done on the advice of the dentist.
For further information: Medicines for the Treatment of GingivitisGingivitis treatment: the role of nutrition
Sometimes, in the therapeutic management of gingivitis, nutrition is also very important: this is the case, for example, of gingivitis favored by vitamin or calcium deficiencies.
and limit / avoid alcohol consumption;