Definition
Cushing's syndrome is the result of chronic exposure to elevated cortisol levels, resulting from excessive administration of corticosteroids or endogenous hypercortisolism. Cusching's syndrome is a serious disease, although fortunately rather rare.
Causes
In the vast majority of cases, Cushing's syndrome is an expression of excessive and prolonged exposure to steroid-based drugs; other subjects develop the syndrome due to an endogenous hyperproduction of cortisol, the result, in turn, of related tumors. pituitary gland, lung cancer (ACTH dependent Cushing syndrome), adrenal adenoma and adrenal carcinoma (ACTH independent Cushing syndrome).
Symptoms
The clinical and symptomatic picture of Cushing's syndrome is expressed in: amenorrhea, skin thinning, weight gain, increased risk of infections, depression, diabetes mellitus, decreased muscle mass, full moon face, hypertension, cardiac hypertrophy, hirsutism, impaired glucose tolerance, obesity, osteoporosis, infant growth retardation, metabolic syndrome, skin ulcers.
The information on Cushing's Syndrome - Cushing's Syndrome Medicines is not intended to replace the direct relationship between health professional and patient. Always consult your doctor and / or specialist before taking Cushing's Syndrome - Medicines to Treat Cushing's Syndrome.
Medicines
The goal of treatment for Cushing's syndrome is to restore cortisol levels in the body to normal; clearly, the best treatment option depends on the nature of the etiopathological agent.
When Cushing's syndrome is favored by chronic and excessive exposure to cortisones (systemic administration of steroid drugs), the endocrinologist will most likely propose a reduction in the dosage.
To understand: some diseases, such as severe asthma or rheumatoid arthritis, require prolonged administration of corticosteroids, which could favor the onset of Cushing's syndrome. In other pathological conditions it is not possible to reduce the dose of corticosteroids, as such an intervention would aggravate the underlying pathology.
It is recommended not to suddenly stop administering steroid drugs on your own initiative. In some patients, the reduction of the corticosteroid dose is not possible: in this case, the patient will have to undergo regular medical checks regarding blood glucose, bone density and cortisol levels, and possibly undergo surgery.
Cushing's syndrome subordinated to the overproduction of ACTH due to pituitary tumors should generally be treated with surgical removal of the tumor and post-surgical radiotherapy; probably, following these interventions, replacement therapy with hydrocortisone may be required, to be taken throughout. life in order to ensure the body the right dose of steroid hormones.
Generally speaking, Cushing's syndrome is often treated with surgery; before undergoing the operation, the patient must normally undergo drug therapy, in order to improve the characteristic signs and symptoms, minimizing the risk incurred during the operation.
Let's see below which drugs are used in therapy to control the secretion of adrenal steroid hormones.
The following are the classes of drugs most used in the therapy against Cushing's syndrome, and some examples of pharmacological specialties; it is up to the doctor to choose the most suitable active ingredient and dosage for the patient, based on the severity of the disease, the state of health of the patient and his response to treatment:
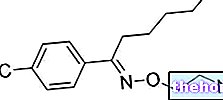
- Ketoconazole (eg. Ketoconazole EG): the recommended dose for the treatment of Cushing's syndrome ranges from 400 to 1200 mg per day, depending on the severity of the symptoms.
- Mitotane (eg Lysodren): this drug is particularly suitable for the treatment of inoperable adrenocortical carcinoma, which reflects Cushing's syndrome. It is a powerful drug, able to selectively inhibit the action of the adrenal cortex: according to this, it is understood that a costicosteroid replacement treatment is necessary following the administration of the drug. It is recommended to start therapy with a dose of mitotane of 2-3 g per day, evenly distributed over the 24 hours.After 8 weeks of treatment, it is recommended to reduce the dose to 1-2 grams / day.
- Dexamethasone (eg Decadron, Soldesam): it is an inhibitor of pituitary secretion that does not have mineralocorticoid action. The long duration of action of this drug is suitable for suppressing ACTH secretion in the context of familial adrenal hyperplasia. Normally, the recommended dosage of this drug is 1 mg, to be taken orally in the evening, to inhibit ACTH secretion. Consult your doctor. Administration of this drug is recommended in the evening, since, being a glucocorticoid, it exerts its suppressive action at the level of the hypothalamus-pituitary-adrenal axis in a more prolonged and intense way during this period of the day.
- Betamethasone (eg Celestone, Bentelan, Diprosone): this drug, just like the previous one, is an inhibitor of pituitary secretion, almost completely devoid of mineralocorticoid action. Administer the drug in the evening. The dosage should be established by the doctor on the basis of the cortisol values in the blood.
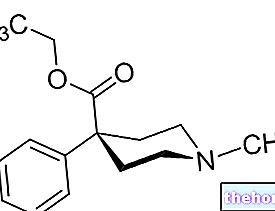
- Metyrapone (Metopirone): the drug, belonging to the class of inhibitors of the adrenal cortex, is not marketed in our country; however, where its use is permitted, metyrapone is used to control the symptoms that characterize Cushing's syndrome, especially before subjecting the patient to surgery for the treatment of the disease. Indicatively, for Cushing's syndrome , take 0.25-6 grams of drug per day, based on cortisol values Consult your doctor.