Definition
In contrast to leukocytosis, leukopenia identifies a clinical condition in which the amount of white blood cells falls below the normal range; in other words, leukopenia delineates an abnormal reduction of leukocytes in the blood.
Leukopenia differs on the basis of the type of cells involved: we remember, in fact, that white blood cells are classified into neutrophils, basophils and eosinophils.
- Leukopenia → number of white blood cells <3500 units / microliter of blood
- Neutropenia → n ° of neutrophils <500-1500 units / microliter of blood
- Eosinophilopenia → number of eosinophils <40 units / microliter of blood
- Basophylopenia → no. Of basophils <10 units / microliter of blood
Causes
Often, leukopenia is an immediate response of the body to bacterial insults or acute inflammatory processes; however, the reduction of leukocytes can result from: megaloblastic anemia, rheumatoid arthritis, deficiency of vitamin B9, copper and zinc, dengue, hepatitis B, drugs antibiotics, diuretics, steroids, immunosuppressants, immunodeficiency, hyperthyroidism, leukemia, lupus, malaria, radiation, sarcoidosis, sepsis, tuberculosis.
Symptoms
Neutropenia is the most common form of leukopenia, and is characterized by symptoms such as mouth ulcers, pharyngitis, fever, pain, recurrent infections (especially staphylococci), enlarged lymph nodes, sepsis, stomatitis. The vast majority of patients with leukopenia have, in general, a high risk of contracting serious infections.
The information on Leukopenia - Drugs for the Treatment of Leukopenia is not intended to replace the direct relationship between health professional and patient. Always consult your doctor and / or specialist before taking Leukopenia - Drugs to Treat Leukopenia.
Medicines
Since leukopenia exaggeratedly increases the risk of bacterial and viral infections, patients who record an "alteration of the leukocyte count, even sensitive, should pay particular attention to primary prevention of infectious diseases, periodically undergoing specific vaccinations. All affected patients. from leukopenia, they should also take care of their personal hygiene and hands, wear a mask to protect themselves from pathogenic insults and not get close to the sick.
The medical-pharmacological therapy is subordinated to the triggering etiopathological element; for example, in some cases, the plasma reduction of leukocytes is compromised by the administration of potent drugs; it is deduced that the suspension of the drug and the replacement of the same with an active drug similar reduces the symptoms, bringing the white blood cell count back to normal.
Generally speaking, a simultaneous bacterial infection is observed in patients with leukopenia: for this reason, the administration of antibiotics is one of the most effective therapies to remove collateral symptoms. Only in cases of extreme severity, it is necessary to intervene with drugs to stimulate the synthesis of white blood cells and the administration of immunoglobulins (antibodies) derived from blood transfusions.
If the cause of the leukopenia depends on cancer or leukemia, the patient will have to undergo one or more chemotherapy courses.
The following are the classes of drugs most used in the therapy against leukopenia, and some examples of pharmacological specialties; it is up to the doctor to choose the most suitable active ingredient and dosage for the patient, based on the severity of the disease, the state of health of the patient and his response to treatment:
Antibiotic drugs for the treatment of infections in the context of leukopenia
In the context of leukopenia, the intake of broad spectrum antibiotics in patients with high fever is indispensable; Often it is preferable to administer these drugs intravenously even before identifying the specific pathogen. If the alteration of the body temperature persists after the first 72 hours from the beginning of the antibiotic therapy, in all probability, the leukopenia does NOT depend on bacterial infections; therefore, the patient must undergo further diagnostic tests.
The most important antibiotic drugs and first-line specialty medicines are listed below.The posology cannot, however, be reported: it is up to the doctor to decide the optimal dosage for that patient, on the basis of the triggering etiological agent; analogous discourse for the duration of therapy.
- Vancomycin (eg Zengac, Levovanox, Maxivanil), glycopeptide class
- Amphotericin B (eg Abelcet), polyene drug indicated for the treatment of fungal infections in the context of leukopenia
- Aciclovir (eg. Aciclovir, Xerese, Zovirax): indicated for the treatment of leukopenia in the context of chicken pox or infections caused by the Herpes simplex virus
- Piperacillin (eg Limerik, Picillin, Ecosette): the drug is a semi-synthetic penicillin, with a broad spectrum of action, indicated for bacterial infections in the context of leukopenia
- Trimethoprim-sulfamethoxazole (eg Bactrim), sulfonamide antibiotic. The drug should be considered in therapy for the prevention of pneumonia in leukopenic patients who do NOT have fever. The drug appears to reduce the frequency of bacterial infections.
Medicines to reduce the secondary symptoms of leukopenia
Oral canker sores and oropharyngeal ulcerations in general are very frequent in patients with leukopenia. To relieve discomfort, it is recommended to take local anesthetic drugs, topical corticosteroids and specific gargling. Here are some examples:
- Benzocaine (eg Foille)
- Benzydamine (eg Difflan)
- Chlorhexidine (eg. Disinfene cream, Golasan mouthwash)
- Nystatin (e.g. Mycostatin) for Candida albicans co-infections in the oral cavity, including in patients with leukopenia
For further information and dosage: read the article on drugs for the treatment of oral canker sores
Medicines to rebalance the concentration of white blood cells in the blood
The administration of the drugs described below is indicated to treat the most common form of leukopenia (neutropenia), both in the variant dependent on chemotherapy and in that associated with HIV infections.
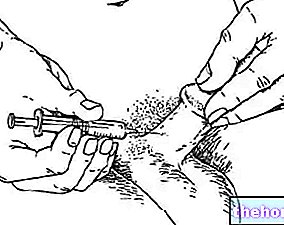
- Filgrastim (eg. Zarzio, Tevagastrim, Filgrastim Hexal, Biograstim, Nivestim): for the treatment of the neutrophilic variant of leukopenia associated with chemotherapy treatments, it is recommended to start therapy with a drug dose of 5 mcg / kg, subcutaneously or intravenously, once a day, for max. 2 weeks (until a neutrophil count of 10,000 units / microliter of blood is reached). Administer 24 hours after chemotherapy. If necessary, increase the dose by 5 mcg / kg per day in case of no response after 5-7 days. For the treatment of leukopenia (var. Neutrophilia) associated with AIDS, it is recommended to take the drug at a dose of 1-5 mcg / kg subcutaneously or intravenously, once a day. If no improvement is observed after 5-7 days, increase the dose by another 5 mcg / kg.
- Pegfilgrastim (eg. Neulasta): the drug is used in therapy to reduce the duration of neutropenia and the incidence of its febrile variant. The drug is available in syringes and pre-filled pens (each dose consists of 6 mg of drug) : administer the drug subcutaneously Consult your doctor for more information.
Corticosteroid drugs: indicated for the treatment of leukopenia in patients with evident increase in cell turnover, expression of autoimmune diseases.
- Prednisone (eg Deltacortene, Lodotra): administered at a dose of 0.5-1 mg / kg per day (every other day), this drug appears to improve white blood cell counts (especially neutrophils) in patients with leukopenia.