
What is Jentadueto?
Jentadueto is a medicine that contains the active substances linagliptin and metformin hydrochloride. It is available as tablets (2.5 mg / 850 mg and 2.5 mg / 1 000 mg).
What is Jentadueto used for?
Jentadueto is used in adults with type 2 diabetes to improve the control of blood glucose (sugar) levels. It is used in addition to diet and exercise in the following ways:
- in patients who are not satisfactorily controlled on metformin (an antidiabetic medicine) used alone;
- in patients already taking a combination of linagliptin and metformin as separate tablets;
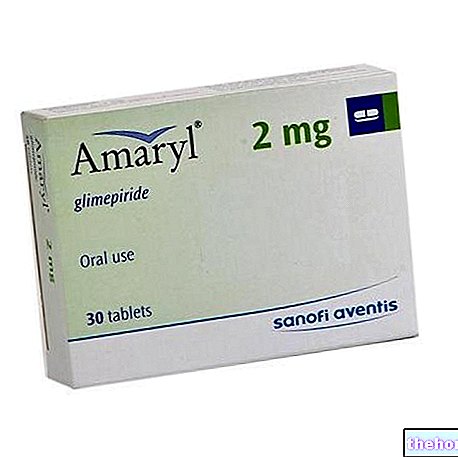
- in combination with a sulfonylurea (another type of diabetes medicine) in patients who are not satisfactorily controlled on this medicine and metformin.
The medicine can only be obtained with a prescription.
How is Jentadueto used?
Jentadueto is taken twice a day. The strength of the tablet to use depends on the dose of the other antidiabetic medicines the patient was taking before. If Jentadueto is taken with a sulphonylurea, the dose of the sulphonylurea may need to be lowered to avoid hypoglycaemia (low blood sugar levels).
The maximum dose is 5 mg of linagliptin and 2,000 mg of metformin per day. Jentadueto should be taken with meals to avoid any stomach problems caused by metformin.
How does Jentadueto work?
Type 2 diabetes is a disease in which the pancreas does not make enough insulin to control the level of glucose in the blood or where the body is unable to use insulin effectively. The active substances in Jentadueto, linagliptin and metformin hydrochloride, each have a different mode of action.
Linagliptin is a dipeptidyl peptidase 4 (DPP-4) inhibitor. It works by inhibiting the breakdown of "incretin" hormones in the body. These hormones are released after food and stimulate the pancreas to produce insulin. By prolonging the action of incretin hormones in the blood, linagliptin stimulates the pancreas to produce more insulin when blood glucose levels are high. Linagliptin does not work if blood glucose is low. Linagliptin also reduces the amount of glucose produced. from the liver by increasing insulin levels and reducing levels of the hormone glucagon. Together, these processes reduce blood glucose levels and help control type 2 diabetes. Linagliptin has been authorized in the European Union (EU) since 2011 under the name of Trajenta.
Metformin works primarily by inhibiting the production of glucose and reducing its absorption in the intestine. Metformin has been available in the EU since the 1950s.
As a result of the action of both active ingredients, blood glucose levels are reduced and this helps to control type 2 diabetes.
How has Jentadueto been studied?
The effects of Jentadueto were first tested in experimental models before being studied in humans.
The company presented the results of four studies with linagliptin in patients with type 2 diabetes, which were used to support the approval of Trajenta in the EU and which compared linagliptin, given at 5 mg once daily, with placebo (a dummy treatment). The studies looked at the efficacy of linagliptin used alone (503 patients), in combination with metformin (701 patients), with metformin plus a sulphonylurea (1 058 patients) or with pioglitazone, another antidiabetic medicine (389 patients).
A new study involving 791 patients with type 2 diabetes was conducted in which the combination of linagliptin plus metformin given twice daily was compared with metformin alone, linagliptin alone or placebo. Linagliptin was administered at a dose of 2.5 mg twice daily in the combination treatment and 5 mg once daily in the single treatment. Metformin was given at a dose of 500 mg or 1 000 mg twice daily, either in combination or single treatment.
An additional study was conducted involving 491 patients with type 2 diabetes taking metformin twice daily, in which placebo or linagliptin at a dose of 2.5 mg twice daily or 5 mg once a day. The study compared the effects of adding linagliptin to metformin in these ways, since metformin must be taken at least twice a day.
In all studies, the main measure of effectiveness was the change in blood levels of a substance called glycosylated hemoglobin (HbA1c) after 24 weeks of treatment. This provides an indication of how well the blood glucose is controlled.
What benefit has Jentadueto shown during the studies?
Studies with linagliptin showed that it was more effective than placebo in lowering HbA1c levels. Used alone, linagliptin gave a reduction of 0.46 points compared with an increase of 0.22 points. Given in combination, linagliptin with metformin gave a reduction of 0.56 points compared with an increase of 0.10 points; linagliptin with metformin plus a sulphonylurea gave a reduction of 0.72 points compared to 0.10 points.
The study with the combination of linagliptin and metformin showed that it was more effective than linagliptin or metformin alone, as well as placebo, in lowering HbA1c levels. The combination gave a reduction of 1.22 points when metformin was given at a dose of 500 mg and a reduction of 1.59 points when metformin was given at a dose of 1000 mg. This compared to a reduction of 0.45 with linagliptin alone, 0.64 with 500 mg of metformin alone, 1.07 with 1000 mg of metformin alone, and 0.13 with placebo.
The study that observed adding linagliptin at a dose of 2.5 mg twice daily or 5 mg once daily to metformin showed a similar reduction in HbA1c levels compared to placebo (0.74 and 0.80 points more than placebo).
What is the risk associated with Jentadueto?
The most frequent side effect of the combination of linagliptin plus metformin was diarrhea (seen in less than 1% of patients, with a similar rate seen in patients taking metformin plus placebo). When linagliptin and metformin were administered with a sulphonylurea, the most frequent side effect was hypoglycaemia observed in approximately 23% of patients compared with approximately 15% when placebo with metformin and a sulphonylurea was given. For the full list of side effects reported with Jentadueto, see the package leaflet.
Jentadueto must not be used in people who may be hypersensitive (allergic) to linagliptin, metformin or any of the other ingredients. It must not be used in patients who have diabetic ketoacidosis or diabetic pre-coma (a dangerous condition that can occur in diabetes), patients with moderate to severe kidney problems or who have acute (sudden) conditions that can have effects on kidney function, patients suffering from acute or chronic diseases that can cause tissue hypoxia (in which the tissues do not have an adequate supply of oxygen) such as heart failure or difficulty in breathing and patients with liver problems, alcohol intoxication or alcoholism. For the full list of restrictions, see the package leaflet.
Why has Jentadueto been approved?
The CHMP concluded that the combination of linagliptin and metformin was shown to be effective in lowering HbA1c levels and that linagliptin at 2.5 mg twice daily was as effective as 5 mg once daily. per day, approved in the EU for use alone and in combination with metformin and metformin plus a sulphonylurea. The CHMP noted that fixed dose combinations may increase the likelihood that patients will take the medicine correctly. Regarding the undesirable effects, the Committee considered that in general the risks found were only slightly greater than those seen with placebo. The CHMP therefore decided that Jentadueto's benefits are greater than its risks and recommended that it be given a Marketing Authorization for the medicine.
More information about Jentadueto
On 20 July 2012, the European Commission issued a "Marketing Authorization" for Jentadueto, valid throughout the European Union.
For the complete version of Jentadueto's EPAR, consult the Agency's website: ema.Europa.eu/Find medicine / Human medicines / European public assessment reports. For more information about Jentadueto therapy, read the package leaflet (included with the EPAR) or contact your doctor or pharmacist.
Last update of this summary: 06-2012.
The information on Jentadueto published on this page may be out of date or incomplete. For a correct use of this information, see the Disclaimer and useful information page.












.jpg)











