Watch the video
- Watch the video on youtube

Skin Fungi - Pityriasis Versicolor
Also called mycetes, fungi are commonly present in the skin flora and in the environment, but generally do not pose a problem; in fact, they tend to "coexist" with the human organism in the saprophytic state, without causing harm. All this thanks to several defensive factors that protect the human body from their excessive development.
In some favorable conditions, however, cutaneous fungi can turn into invasive pathogens, behaving like opportunistic microorganisms. In practice, these fungi are capable of “exploiting” a weakened immune state of the organism to increase their colonies on the skin, to the point of causing disease.
Not surprisingly, infections caused by skin fungi are found more frequently during the summer, when the heat and humidity typical of the summer season facilitate their growth and spread among individuals (given the frequentation of crowded places, such as swimming pools and beaches).
The symptoms associated with mycosis of the skin manifest themselves in the skin sites and in the attached structures (eg scalp, nails, genitals or skin surface) that they infect.
Epidemiology varies from one form of mycosis to another and is largely influenced by multiple environmental and subjective factors.
The diagnosis is based on the clinical appearance of the lesions, detected at the dermatological examination, and on the microscopic and cultural examination of the infected tissue.
Treatment depends on the site of infection, but generally involves the use of topical or oral antifungals, aimed specifically at the skin fungus in question.
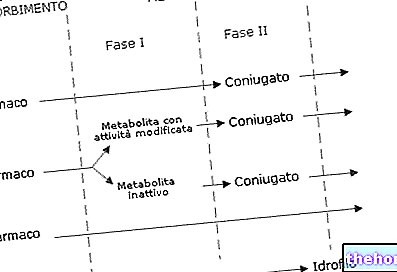
of plants or animals. Mycology experts are able to identify and classify fungi based on their microscopic appearance and method of reproduction, which can occur both sexually and asexually. The fungi that infect human skin are microscopic in size and can be single-celled with an ovoid shape (like yeasts) or multicellular and filamentous (like molds).Species belong to this category Epidermophyton, Microsporum And Trichophyton.
Dermatophytes are responsible for characteristic rosette-shaped, sharp-edged skin macules with centrifugal evolution (ringworm). Some of these fungi can infect the trunk (tinea corporis), feet (tinea pedis or athlete's foot), nails (tinea unguium) and inguinal folds (tinea cruris). These infections make up about 40-50% of all. superficial mycoses and differ from candidiasis in that they are only rarely invasive.

Skin Fungi - Tinea Pedis (Athlete's Foot)
- Yeasts: they are single-celled and non-filamentous microorganisms that reproduce very quickly in an asexual way, localizing in warm-humid areas of the body (oral cavity, armpits, submammary folds, interdigital spaces, anogenital region, etc.).
Many yeasts are normally present on the skin and do not cause damage (they almost always coexist in a saprophytic state).
The most important yeasts in dermatology are: Candida albicans, Malassezia furfur And Cryptococcus neoformans.
Depending on the fungal agent responsible and the affected area of the body, visible skin manifestations may include edema, redness and pinkish-white desquamative patches; itching is almost always present. - Molds: are multicellular and filamentous fungi that reproduce sexually.
The most common pathogenic molds are: Alternaria, Aspergillus And Fusarium. These types of fungi are mainly responsible for deep and systemic mycoses, while only in rare cases they cause skin and superficial infections.
In general, these pathologies can be divided into two types:
- Superficial and cutaneous: limited to the superficial layer of the skin (epidermis), hair, nails and mucous membranes (oral cavity and genitals);
- Subcutaneous: extended to the dermis and connected structures.
Skin diseases due to fungi can affect everyone, regardless of gender and age. In most cases, people who develop cutaneous mycosis have a reduced immune response, for example due to an "alteration of local defenses (eg trauma with vascular compromise) or" immunosuppression (eg diabetes, AIDS, antibiotic dysbiosis, etc.).
Transmission can occur from person to person, from animal (cat, dog, rabbit, mouse and cattle) to person and, rarely, from contaminated soil and objects to humans.
The most frequent fungal infections of the skin are:
- Dermatophytosis: Fungal infections involving keratinized areas of the body (stratum corneum, hair or nails). Symptoms can vary, but most of the time they are skin lesions, which rarely itch.
- Candidiasis: mycoses that mainly affect sweating areas, such as groin, armpits and interdigital areas. At the level of the mucous membranes, the oral cavity (e.g. thrush), the genitals (e.g. vulvovaginitis from Candida albicans) and the esophagus (especially in immunosuppressed subjects).
- Pityriasis versicolor: fungal skin infection in which small, flat, uneven patches appear on the neck, trunk, abdomen, arms and face.
Characteristic of the disease is the alteration of skin pigmentation (dyschromia): the lesions are hypo- or hyper-pigmented and take on a color ranging from white to brown. The colonized skin areas, in fact, if exposed to the sun, hinder the passage of ultraviolet rays which, in normal conditions, stimulate the production of melanin.
These conditions include:
- Wrong eating habits;
- Insufficient hygiene;
- Physical stress;
- Hot and excessive humidity;
- Situations of chronic skin maceration (excessive sweating, habit of wearing poorly breathable clothing);
- Prolonged antibiotic or cortisone-based therapies;
- Immune defense compromised by particular pathologies (AIDS, tumors, diabetes, etc.);
- Taking immunosuppressive drugs.
In some fungal infections, the lesions are whitish first, then tend to darken over time.
Most of the time, the inflammation is little or no, but occasionally when the inflammation is more severe it involves damage to the structures involved, manifesting as a sudden blistering or bullous disease (usually in the feet) or as a "large soft lesion of the scalp that results in areas of alopecia (kerion).
Other symptoms associated with skin fungus include a burning sensation, sudden onset blisters and cracks (especially in the feet), thickening of the nails and dandruff-like scaling of the scalp.
For the differential diagnosis, the doctor can also use the Wood's lamp, able to detect a typical fluorescence (e.g. golden yellow of the Malassezia, greenish for dermatophytes, etc.) and exclude these dermatosis infections not caused by fungi.
Once the type of skin fungus responsible for the clinical symptoms has been identified (through culture), the doctor can prescribe a specific therapy.
topicals (such as hydrocortisone). Oral corticosteroid drugs are rarely used to treat severe inflammatory lesions.
For further information: Drugs for the treatment of mycosis of the skin », modify the pH of the skin and favor the stagnation of humidity.